EAPCI Textbook High Yield Boxes
Thrombectomy and target vessel protection during PCI
- Coronary embolization phenomena can spontaneously occur and are frequent during PCI, significantly contributing to MVO and carrying prognostic implications
- Coronary embolization phenomena can spontaneously occur and are frequent during PCI, significantly contributing to MVO and carrying prognostic implications
- Coronary micro-embolization is not always angiographically evident, but MVO can be suspected by intracoronary imaging and functional invasive assessment and visualized by post-procedural non-invasive techniques, among which contrast MRI has nowadays a leading role.
Ostial lesions
Indications for ostial PCI and lesion evaluation> Indications:
- Unstable angina pectoris
- Other acute coronary syndromes
- Stable, effort induced angina pectoris or dyspnoea (angina equivalent)
- Significant territory of ischaemic myocardium at risk (can be anticipated in aorto-ostial disease)
>Evaluation:
- Lack of contrast reflux or significant pressure drop/ventricularisation after intubation with the guide catheter (CAVE: ostial spasm, non co-axial alignment)
- Intravascular ultrasound (IVUS) and fractional flow reserve (FFR) (CAVE: guide catheter disengagement required)
- Quantitative coronary angiograph (QCA) (CAVE: no proximal reference)
Technical considerations in ostial PCI
- Aorto-ostial lesions are often rigid and calcified
- Catheters with less support (e.g., Judkins shape) or short-tipped versions may be preferrable
- DES are preferred due to better clinical outcomes
- Guide catheter positioning in aorto-ostial lesions is critical to avoid occlusion of the vessel, vessel dissection, and for precise stent positioning
- Consider the use of debulking techniques for rigid and heavily calcified ostial lesions
- Achieve full stent coverage of the ostium without unnecessary extension into the aorta or main vessel
- Choose appropriate angiographic views without foreshortening or overlap of the ostium
- Post-dilatation: after stent implantation routine high-pressure post-dilatation with non-compliant balloons is highly recommended
Saphenous vein graft disease
Natural history of vein graft disease- Thrombosis
- early phenomenon, related to vein damage and technical issues
- about 10% of vein grafts are occluded and are frequently asymptomatic in the first month after CABG - Intima hyperplasia
- occurrs in the first months after CABG
- represents the basis for later atherosclesosis - Atherosclerosis
- dominant disease process involving the vein graft after 1 year
- usually symptomatic for 3 years after CABG
- morphologically characterised by diffuse, concentric, and friable plaques with a poorly developed or absent fibrous cap and little evidence of calcification
Specific graft lesion intervention subtypes and the related outcomes
- Early ischaemia after CABG surgery (within the first 30 days)
- early graft occlusion, usually thrombotic, occurs in up to 10%
- 3% to 6% of patients develop clinically significant ischaemia
- in symptomatic patients, 37% to 56% SVG are occluded on angiogram
- PCI is recommended in the presence of clinical evidence of relevant ischaemia - Stenosis of the distal anastomosis
- PCI has particularly good results, better than ostial and shaft location results - Internal mammary artery graft disease
- balloon PCI appears to be the procedure of choice to treat internal mammary artery stenosis - Chronic totally occluded SVG
- related to poor short-term and long-term outcomes
- native recanalisation is preferred if possible
- PCI only justified in the presence of life-impaired symptoms or a large, jeopardised myocardium
Drug-eluting stents (DES) versus bare metal stents (BMS) to treat saphenous vein grafts
- DES have shown to be more effective that BMS by reducing the rate of TLR
- Initial concern about DES safety was raised by the long-term follow-up of a small-randomised trial
- Long-term safety of DES is supported by a large amount of data coming from large real-world series
Strategies to prevent no-reflow in SVG interventions
- Pharmacology
- glycoprotein IIb/IIIa inhibitors increase the rate of bleeding without any apparent benefit
- vasodalitors can improve angiographic results but do not appear to improve clinical outcomes - Covered stents
- their use has been linked to worse outcomes in several randomised trials
- use not recommended - Embolic protection devices
- strategy that might decreases periprocedural myocardial infarction and the no-reflow phenomenon
- routine use is recommended in selected high-risk interventions
- both proximal and distal protection devices should be available and used according to disease location in the graft itself - Direct and undersized stenting
- alternative approach to prevent distal embolization
Acute myocardial infarction due to saphenous vein grafts
- High related in-hospital mortality and poor long-term prognosis
- Possible role of aspiration thrombectomy – especially in the presence of visible thrombus
- Possible role of staged procedure after aggressive pharmacology approach
Risk stratification and risk models in revascularisation
The Global Risk Classification matrix [12]
- Global Risk Classification (GRC) is derived using the above matrix
- The GRC divides patients into Low, Intermediate and High-risk groups as shown
Interventions for stable coronary disease (chronic coronary syndromes)
Typical assessment of severity of stable CAD- Anginal Symptoms
- Ischaemia on stress testing and FFR measurement
- Anatomical disease by coronary angiography and IVUS
Increased adverse clinical events, including MI and death, are associated with patients presenting with severely limiting angina, significant ischaemia on stress testing or FFR measurement, and multivessel CAD
Proven Benefits of PCI in patients with stable CAD
- Relieve anginal symptoms
- Reduce ischaemic burden
- PCI has not been shown to reduce MI or death in patients with stable CAD. Optimal medical therapy (OMT) has consistently been shown to reduce death, MI, and stroke rates. However, significant reduction in ischaemic burden have been associated with reduced myocardial infarctions and improved survival, and PCI in addition to OMT achieves a greater reduction in ischaemic burden compared to OMT alone. PCI has also been associated with improved regional left ventricular function in patients with hibernating myocardium
Comparisons of PCI versus CABG in patients with stable multivessel CAD
- Outcomes with PCI are comparable to CABG for low complexity CAD
- Outcomes with CABG are superior to PCI for intermediate to high complexity CAD
- Patients treated with PCI with Taxus drug eluting stents in the SYNTAX trial had similar 3 year clinical outcomes as those who underwent CABG if the anatomical complexity of disease was low (by SYNTAX score). However, those with intermediate to high SYNTAX scores had higher 3 year MACCE rates with PCI compared to CABG
Comparisons of optimal medical therapy (OMT), CABG and PCI for treatment of stable CAD
- OMT is necessary in all patients with stable CAD, whether or not they receive revascularisation of any type
- PCI is the preferable method of revascularisation in most patients with single vessel CAD and significant ischemia
- PCI may be reasonable revascularisation strategy compared to CABG in patients with less complex CAD (single vessel CAD and patients with multivessel CAD with low SYNTAX scores/low burden of disease
- CABG is preferable to PCI for multivessel and left main CAD in patients with diabetes or intermediate to high anatomical complexity or SYNTAX scores
- PCI may be a reasonable option for patients with complex CAD, but who are at high risk for complications and mortality with CABG due to other comorbid conditions
- In all cases of choosing revascularisation strategies, a patient centered approach with informed consent about all reasonable options should be taken
Interventions for non-ST-segment elevation acute coronary syndromes
A 12-lead ECG should be obtained within 10 minutes after medical contactThe radial approach reduces the risk of bleeding compared with the femoral approach
Risk and bleeding scores should be used
Aspirin should be given to all patients with NSTE-ACS
All patients with NSTE-ACS should receive either Prasugrel or Ticagrelor unless there are contraindications over at least 12 months
The routine use of GP IIb/IIIa receptor inhibitors is not recommended, see Table 6
Anticoagulation is recommended in all patients with NSTE-ACS. Fondaparinux is the anticoagulant of first choice, see Table 7
Interventions for patients with diabetes mellitus
Pathophysiological substrate in type 2 diabetes mellitus- Insulin resistance and hyperglycaemia provide a substrate for both metabolic dysfunction and a pro-thrombogenic state in type 2 DM
Antiplatelet therapy in diabetes mellitus
- ASA and clopidogrel have been the cornerstone antiplatelet treatment in diabetic patients during the last two decades
- In addition, GP IIb/IIIa inhibitors have also been considered specifically in acute coronary syndromes
- Despite this regimen, clinical events are persistently higher in diabetics as compared to non-diabetics
- Aspirin resistance and clopidogrel response variability may play a role in this regard
- New antiplatelet agents such as prasugrel and ticagrelor are currently the first-line treatment in diabetic with acute coronary syndromes.
Metabolic control in diabetes mellitus
- Glycaemic control is essential to improve long-term outcomes in diabetic patients, especially after revascularisation
- During hospitalisation, refined glucose control is desirable to avoid ominous hypoglycaemia
- New inhibitors of sodium-glucose cotransporter 2 (empagliflozin and dapagliflozin) may play a role in decelerating the progression of atherosclerosis in diabetic patients
Renal complication after contrast administration in diabetic patients
- Diabetes mellitus per se represents a high risk of contrast-induced nephropathy
- Some of the comorbidities commonly seen in diabetics (i.e., previous renal dysfunction) may have a synergistic and detrimental effect on renal function following diagnostic or therapeutic interventions
- Close monitoring of renal parameters and the avoidance of nephrotoxic agents are essential to prevent and treat such complications. In the event of nephropathy, metformin has to be stopped during catheterisation or PCI
Secondary coronary revascularisation
PCI in saphenous vein grafts- Patency rate of SVG is a time-related phenomenon, decreased to 50% at 10 years. SVG late failure is a common scenario for secondary revascularisation.
- Percutaneous interventions in the SVGs are fraught with a number of potential complications, namely the risk of rupture as a result of over-dilatation and the frequent occurrence of athero-embolism.
- The current ESC guidelines recommend to consider PCI via the bypassed native artery over PCI of the bypass graft and DES for all PCI interventions
PCI in native coronary arteries post CABG
- Native coronary vessels in patients with previous CABG have extensive atheromatosis and unfavourable characteristics for PCI such as vessel calcification, left main location and chronic occlusions.
- The main objectives of native vessel treatment after CABG is to restore vessel patency without putting in jeopardy functional grafts.
- In patients with CABG failure, those treated with PCI in native vessels have less rates of in-hospital complications, including mortality, than patients treated with grafts PCI.
Urgent surgery for acute PCI failure
- Currently, the need for urgent surgery due to acute PCI failure is uncommon.
- Most PCI-derived acute complications can be successfully managed in the catheterization laboratory.
- Unsuccessful pericardiocentesis of PCI-derived cardiac tamponade and PCI failure involving a large myocardial territory are the most frequent scenarios for urgent surgery/rescue CABG
CABG for late PCI failure
-
It is unclear from the data if prior PCI definitively increases the risk of adverse outcomes in patients undergoing CABG.
-
A tendency to practice episodic care in coronary revascularisation must be avoided, despite a potential adverse interaction between prior coronary stenting and subsequent need for CABG.
- Symptomatic patients with recurrent or diffuse in-stent restenosis, progressive multivessel disease, previous incomplete revascularisation, and associated complex lesions such as chronic total occlusions should be considered for CABG before repeat PCI.
Role of imaging and intravascular techniques in secondary revascularisation
- MSCT is a valuable tool in the study of patients with prior CABG by helping to locate the grafts, allowing a more selective invasive coronary angiography, and allowing for the assessment of calcified or occluded vessels that are potential PCI targets.
- MSCT provides also important anatomical information for repeat cardiac surgery, such as the relationship of cardiac structures to the sternum. Grafts must be located >10 mm from the sternum to minimize the risks of sternotomy.
- Intracoronary imaging techniques such as intravascular ultrasound and optical coherence tomography allow the assessment of underlying mechanisms which might have contributed to the development of stent failure (i.e. in-stent restenosis and stent thrombosis). This information is very useful to optimise the new PCI procedures.
Hybrid interventions
- In selected patients with multivessel disease hybrid therapy is a realistic approach with good long-term outcome results.
- It offers the advantage of a complete revascularisation while combining the survival benefit of internal mammary artery on the left anterior descending coronary artery and the superior patency rate of (drug-eluting) stents as compared with venous grafts
- Hybrid therapy for patients with combined coronary and (multi)-valvular disease was made possible by progresses in the field of minimally invasive cardiac surgery and trans-catheter techniques.
- No matter the strategy (percutaneous revascularisation and/or transcatheter aortic valve implantation and/or endoscopic valvular surgery), the goal of such an approach is to offer both symptomatic relief and the potential of improved long-term survival with the advantage of a lower periprocedural morbidity and mortality
Cardiogenic shock
Criteria for cardiogenic shock definition- Systolic blood pressure < 90 mmHg lasting >30 minutes (in the absence of hypovolaemia) or vasopressors required to achieve a systolic blood pressure ≥90 mmHg
- Pulmonary congestion or elevated left ventricular filling pressures (pulmonary capillary wedge pressure >18 mmHg)
- Signs of impaired organ perfusion with at least one of the following criteria
a) Altered mental status
b) Cold, clammy skin and extremities
c) Oliguria with urine output <30 ml/h
d) Serum-lactate > 2.0 mmol/l - Reduction of cardiac index (<1.8 l/min/m² without and 2.0-2.2 l/min/m² with support) (optional)
Causes of cardiogenic shock
- Acute myocardial infarction (>40% loss of functional myocardium)
- Mechanical complication of acute myocardial infarction
−−Ventricular septum defect
−−Free wall rupture
−− Acute ischaemic mitral regurgitation (papillary muscular dysfunction) - Acute (peri-) myocarditis
- Apical ballooning syndrome
- Sustained tachyarrhythmias or bradyarrhythmias
- Acute valvular dysfunction
- Intracardiac tumours
- End-stage cardiomyopathies
Mechanisms behind the associations of bleeding/transfusion with mortality
- Hypotension
- Anaemia
- Ineffective oxygen delivery
- Vasoconstriction
- Platelet dysfunction
- Cessation of evidence-based antithrombotic or antiplatelet therapies
Mechanisms of ischaemic mitral regurgitation
- LV global or regional remodelling
- Papillary muscle dysfunction (rare)
- Papillary muscle rupture (partial or complete)
- Acute systolic anterior motion of the mitral valve
Predictors of mortality in cardiogenic shock
- Increasing age (≥75 years)
- Prior infarction
- History of hypertension
- Signs of systemic hypoperfusion not quickly reversible
- Impaired left ventricular ejection fraction (<25%)
- Pulmonary capillary wedge pressure ≥25 mmHg
- Reduced cardiac power index
- Long time from symptom onset to PCI
- Post-PCI TIMI I-flow <3
- Multivessel disease
- High admission blood glucose
- Impaired baseline renal function
- High serum lactate
- APACHE-2 score
The prevention and management of complications during percutaneous coronary intervention
Procedural complication categories [2]- Death (related to the procedure, regardless of mechanism)
- Stroke
- MI (related to the procedure, regardless of mechanism)
- Ischaemia requiring emergency CABG
- Vascular access site complication
- Contrast agent nephropathy
- Excessive bleeding, requiring treatment
- Other (such as coronary perforation and tamponade)
Universal definition of MI
(categories that apply to PCI complications) [8].
- Periprocedural MI1 Type 4a MI >3x 99th percentile* of biomarker
- Stent thrombosis MI2 Type 4b MI based on angiography or autopsy
- CABG MI3 Type 5 MI >5x 99th percentile* of biomarker
1 If cardiac troponin is elevated before the procedure and not stable for at least two samples 6hrs apart, there are insufficient data to recommend biomarker criteria for MI
2 Must meet the criteria for spontaneous MI as well
3 When associated with the appearance of new pathological Q-waves or new LBBB, or angiographically documented new graft or native coronary artery occlusion, or imaging evidence of new loss of viable myocardium
Complications from femoral access for PCI
- Retroperitoneal haemorrhage
- Pseudoaneurysm
- AV fistula
- Infection
- Haematoma
- Neuropraxia
- Lower limb ischaemia (thrombosis or embolism)
- Dissection
Predictors of complications relating to vascular access
- Female gender
- Advanced age
- Small body surface area
- Prior instrumentation
- Anticoagulation
- Peripheral vascular disease
- Diabetes Mellitus
- Suboptimal technique (puncture and closure)
How to reduce transfemoral access complications
- Access using fluoroscopy (or ultrasound)
- Puncture site at or below centreline of the femoral head
- Femoral angiogram (RAO 30 and LAO 60 degrees) prior to closure
- PCI and anticoagulate only if in the ‘safe zone’ (elective patients)
Reported complications from transradial access for PCI
- Vasospasm
- Pseudoaneurysm
- Puncture site granuloma (one brand of hydrophilic sheath use only)
- Dissection
- Perforation/forearm or chest wall haematoma
- Compartment syndrome
How to reduce transradial access complications
- Hydration and anxiolysis
- Vessel “cocktail” (usually calcium channel antagonist and/or nitrate)
- Heparin (at least 3-5000 units)
- Avoid puncture through the flexor retinaculum
- Perfusion haemostasis
Indications for emergency cardiac surgery following PCI [45]
- Extensive coronary dissection (54%)
- Perforation/tamponade (20%)
- Recurrent acute vessel closure (20%)
- Haemodynamic instability (3%)
- Aortic dissection (2%)
- Guidewire fracture (1%)
Physiological parameters that should prompt patient re-evaluation
- Decreased level of consciousness
- Respiratory rate <8 or >30min-1
- SaO2 <90% on room air
- Central systolic BP<90 mmHg or MAP<70 mmHg
- Change in cardiac rhythm
Stent thrombosis
BMS versus DES- Randomised controlled trials, observation studies and meta-analyses have demonstrated increased rates of ST through two to three years follow-up for BMS (versus newer generation DES) with the greatest portion of risk difference favoring DES observed during the first year of follow-up.
- The incidence of ST is increased following PCI for both “off label” indications or in patients with diabetes mellitus regardless of stent type
- The treatment effect (benefit) of longer (30 months) versus shorter (12 months) duration DAPT therapy for ST reduction appears to be consistent for DES and BMS.
DES versus DES
- Rates of ST may differ between currently available DES platforms and are generally higher following deployment of PES
- Large scale randomised trials and meta-analyses of multiple randomised trials have demonstrated lower rates of early, late and very late ST following deployment of XIENCE®/PROMUS® EES, ENDEAVOR®/Resolute ZES and bioresorbable polymer DES
- Data from multiple sources suggest that BMS have a continued low risk for very late ST
Peri-procedural and post-procedural antithrombotic pharmacotherapy
BackgroundTo optimise efficacy of therapy and reduce the potential bleeding hazard both, ischaemic and bleeding risks, have to be evaluated on an individual basis
Stable/elective patients
- Unfractionated heparin and ASA plus clopidogrel are the antithrombotic therapies of choice
- GPIs should only be used in bailout situations elective PCI
Patients with NSTE-ACS
- Ticagrelor (in all NSTE-ACS patients) and prasugrel (in high-risk patients referred for PCI after the coronary anatomy is known) are recommended over clopidogrel
- Pre-treatment of patients with suspected NSTE-ACS is no longer recommended by the updated guidelines
Patients with STEMI
- In primary PCI, unfractionated heparin (UFH) is the first choice as anticoagulant
- Fondaparinux is contraindicated in patients referred for primary PCI (but can be used in patients treated with fibrinolytic therapy or conservatively)
- Prasugrel and ticagrelor have replaced clopidogrel as the first choice therapy
Percutaneous balloon mitral commissurotomy
Choosing Inoue balloon size
IB: Inoue balloon
* It is advisable to start 1 or 2 mm below the initial balloon size if there is very severe mitral stenosis (valve area <0.5 cm²), or severe commissural calcification
How to solve problems when using the Inoue balloon

IB: Inoue balloon
RA: right atrium
LV: left ventricle
Criteria for ending PMC
- Valve area >1 cm²/m² BSA, and
- complete commissural opening in at least 1 commissure, or
- appearance or increase of regurgitation >1+
Special caution is needed in: elderly patients;; very severe stenosis; extensive subvalvular lesions; nodular commissural calcification; if asymmetric mode of opening ; and during pregnancy BSA: body surface area
Management and prevention of embolism during PMC

LAA: left atrial appendage; PCI: percutaneous coronary intervention; PMC: percutaneous mitral commissurotomy
Management and prevention of severe mitral regurgitation during PMC

MR: mitral regurgitation
Management of hypotension during PMC
- Look at ECG:Bradycardia +/- ST elevation: air embolism is likely (specific treatment)
- Look at LA pressure:High V wave: severe MR is likely (specific treatment)
- Look at echocardiography:Tamponade: drainage
Segmental LV dysfunction: coronary embolism (specific treatment)
LA: left atrium; MR: mitral regurgitation
Contraindications to percutaneous mitral commissurotomy
- Mitral valve area >1.5 cm²
- Left atrial thrombus
- More than mild mitral regurgitation
- Severe or bicommissural calcification
- Absence of commissural fusion
- Severe concomitant aortic valve disease, or severe combined tricuspid stenosis and regurgitation
- Concomitant coronary artery disease requiring bypass surgery
Transcatheter mitral valve repair
Mitral regurgitation- Mitral regurgitation (MR) contributes to significant morbidity and mortality.
- In degenerative MR, medical treatment may be insufficient and cardiac surgery has been the only effective option for decades.
- In functional MR, symptoms may be improved by medical treatment and, if indicated, cardiac resynchronization therapy (CRT).
- Transcatheter mitral valve repair techniques are increasingly used and can be an option for those patients who are not suitable for cardiac surgery.
Coronary sinus approach for indirect mitral annuloplasty
- The coronary sinus provides an easily accessible and minimally invasive approach for percutaneous mitral annuloplasty.
- Its main limitation is the indirect relationship of the coronary sinus to the mitral annulus.
- The potential risk of coronary artery compression and device fracture have been issues in early experience human studies with the CarillonTM
- The main advantages of a coronary artery approach are the avoidance of trauma to the native mitral leaflets or chords, and the fact that it does not preclude future mitral therap
- Early clinical results have demonstrated significant MR reduction and clinical benefit; further investigation of the CarillonTM and ARTOTM system is ongoing.
Transcatheter approaches for direct mitral annuloplasty
- Direct annuloplasty overcomes some of the limitations of a coronary sinus annuloplasty, but represents a technically more challenging and complex procedural approach.
- Obtaining good and durable device anchoring without inducing complications is the main challenge of this approach.
- A percutaneous transvenous transseptal approach has now been developed for both the CardiobandTM and MillipedeTM device.
- Early clinical results have demonstrated reduction of MR and clinical benefit – further development and investigation of the CardiobandTM and MillipedeTM device is ongoing.
Transcatheter edge-to-edge mitral valve repair
- The MitraClipTM system is currently the most studied and most used transcatheter mitral valve repair technique.
- Transcatheter edge-to-edge mitral valve repair requires high-quality TEE imaging (including 3D imaging) and is associated with a substantial learning curve.
- Transcatheter edge-to-edge mitral valve repair can be a treatment option for both functional and degenerative severe MR.
- The MitraClip™ system is the only transcatheter mitral valve device, so far, to show improved survival in heart failure patients with functional MR.
Transcatheter mitral valve chordal repair
- Transcatheter, transapical, beating heart, off-pump mitral valve repair.
- To treat severe degenerative MR due to a prolapse or flail mitral valve leaflet.
- The NeoChordTM and HARPOONTM systems are transcatheter mitral valve chordal repair systems currently under investigation.
- Transcatheter chordal repair systems only leave a minimal ‘anatomical footprint’ behind and do not preclude future mitral therap
Balloon aortic valvuloplasty
Aortic stenosis European guidelines- Aortic stenosis is the most frequent valvular disease in the Western world. Its prevalence increases with age
- Current guidelines recommend surgical aortic valve replacement for low-risk patients with severe AS and symptoms, reduced LV function or concomitant heart surgery
- Current guidelines recommend TAVI in patients with severe AS and symptoms, if inoperable or at high-risk for surgery. TAVI is also an alternative for surgery in intermediate-risk patients when a transfemoral approach is feasible.
Techniques of balloon aortic valvuloplasty
- BAV has become simple and quite safe.
- It is performed under local anaesthesia using the common femoral retrograde approach using standard catheterisation technique
- Balloon inflation is performed under rapid ventricular pacing so as to stabilise the balloon across the aortic valve
BAV results
- BAV is successful in reducing the transvalvular gradient, improving symptoms and left ventricular ejection fraction
- The restenosis rate is high, close to 80% at one year and BAV does not improve survival when performed as a stand-alone procedure
BAV complications
- With improved technique and operator skills, complications are rare
- Massive aortic regurgitation occurs in less than < 2%
BAV indications in the TAVI era
- There is an increasing role of BAV as a bridge to surgical aortic valve replacement or TAVI in patients who present with temporary contra-indications
- Pre-dilatation is performed as the first step of the TAVI procedure
- Non compliant balloons may be also used for post dilatation of balloon-expandable prosthesis at the exact diameter. Post-dilatation may be also performed in order to reduce the severity of residual paravalvular leak after balloon or self-expandable prosthesis.
Percutaneous pulmonary valvuloplasty
Indications for balloon pulmonary valvuloplasty in neonates and children- Neonates : Symptomatic valvar pulmonary stenosis
- Transvalvular gradient <40mmHg acceptable in presence of low cardiac output or with patent arterial duct and a right to left shunt - Children : Moderate or severe valvar pulmonary stenosis irrespective of symptoms
- Transvalvular gradient>40mmHg with normal resting cardiac output
- Elective at 9-12months if asymptomatic
Indications for balloon pulmonary valvuloplasty and surgery in adults
- Valvar pulmonary stenosis with an echocardiographically assessed transvalvar gradient of > 64 mmHg
- If balloon valvulopalsty is ineffective, surgery should be considered in asymptomatic patients with a transvalvar gradient gradient of >80mmHg
- Balloon valvuloplasty can be considered in patients with a transvalvar gradient of > 64 mmHg and
- symptoms related to valvar pulmonary stenosis
- impaired right ventricular function
- double-chambered right ventricle
- relevant arrhythmias
- right to left intracardiac shunting
Balloons and materials for balloon pulmonary valvuloplasty
- Ideal balloon diameter for effective dilatation of valvar stenosis is 110-120% of the annular dimeter measured in echo
- Balloon length should be chosen to facilitate stability during inflation. Length should be at least 1.5 times of the diameter
- Valvar balloon dilatation does not require high-pressure balloons and can be successfully achieved with low pressure inflation
- The most commonly used balloons are NuMed and Balt because these companies offer a large range of available balloon types and sizes.
- In children and neonates, an effort needs to be made to use balloons with low profile to insure an acceptable size of vascular access
- In bigger children and adults, a stiff exchange support wire of 0.035-0.038” is required. In smaller children and neonates, smaller wires tpically of 0.018” are used to support low profile balloons
Percutaneous pulmonary valve implantation
Clinical and morphological requirements for PPVI using the MelodyTM device- Clinical indications in the context of RV pressure overload/pulmonary stenosis:
−RV systolic pressure > 65% of systemic pressure in symptomatic patients
−RV systolic pressure > 75% of systemic pressure in asymptomatic patients - Clinical indications in the context of RV volume overload/pulmonary regurgitation:
−Severe pulmonary regurgiation on echocardiography or MR imaging and
−Severe RV dilatation > 150 ml/m2 or the RV to LV end-diastolic ratio of > 1.7 and/or
−Rapid progressiv RV dilatation and/or
−Severe RV dysfunction and/or
−Symtoms and/or
−Sustained atrial or venticular arrhythmia and/or
−Impaired exercise capacity (<65% compared to norm peak oxygen consumption)
Assessment of RVOT shape and dimensions prior to PPVI
- 3-dimensional shape of the RVOT and pulmonary bifurcation
→ MR whole heart imaging and/or MR angiography - Minimal and maximal diameter diameter of the implantation site
→ Measurements on 2 orthogonal MR cine images through the RVOT - In case of borderline RVOT dimensions on MR
→ Use of sizing balloons during catheterisation - Assessment of RVOT distensibility
→ Use of sizing balloons during catheterisation
Assessment of risk of coronary compression during and after PPVI
- In all patients
−Coronary artery anatomy and proximity to the RVOT judged on MR whole heart imaging and/or MR angiography
−Aortic root angiography in AP and lateral projection - In case of any doubts
−Simultaneous high-pressure balloon inflation within the RVOT and selective coronary angiography
Atrial septal defect and patent foramen ovale closure
Atrial septal defect- 10% of patients with congenital heart disease have an atrial septal defect (ASD)
- Different types of ASD can be differentiated by TEE:
- Secundum ASD: 80% of ASDs, located in the region of the fossa ovalis and its surroundings
- Primum ASD: 15% - Diagnostic cardiac catheterisation is required for percutaneous closure of the ASD and for clarification of non-conclusive non-invasive results
- The success rate for percutaneous closure of secundum ASDs is very high with a complete closure rate of more than 95%
- The risk of complications with device closure of secundum ASDs is low with a frequency of less than 0.5%
- Antiplatelet therapy is usually given for 3-6 months with a minimum of 100 mg aspirin daily
Patent foramen ovale
- Patent foramen ovale (PFO) is associated with cryptogenic ischaemic events
- Detection of PFO is usually performed by TEE or TTE
- Stroke is a leading cause of death and the leading cause of long-term disability
- The presence of an atrial septal aneurysm (ASA) is more frequent in patients with cryptogenic stroke compared to the general population
- Patients with platypnoe orthodeoxia are also linked to PFO
- The presence of a PFO increases the probability of decompression illness
- Several devices are approved for PFO closure in Europe
- Most of the devices have a double umbrella design
Ventricular septal defect closure
Congenital muscular VSDMuscular VSD closure can be performed in children weighing more than 5 kg. In smaller children a hybrid approach is a safer alternative
Complete heart block and perimembranous VSD closure
Risk of complete atrioventricular block in perimembranous VSD device closure is higher in children aged <6 years
Transcatheter residual VSD closure
- Transcatheter closure of residual VSD should be considered as a first choice treatment. Because of anatomical variations many tips and tricks (defect sizing, retrograde transaortic approach, opening of the left device disc in the ascending aorta) may be needed in order to succeed
Post-myocardial infarction VSD
-
Post-myocardial infarction VSDs are associated with a 97%-99% one-year mortality rate. Surgical procedures have a one-month mortality of 50%-60%
- Transcatheter device closure has a similar mortality rate in the early phase. Two to four weeks after myocardial infarction or in the case of residual defects after surgical patch repair, the transcatheter approach can be considered the first-choice treatment
Patent ductus arteriosus closure
Complications- Embolisation of PDA closure
- Aortic or pulmonary vein stenosis
- Haemolysis
Left atrial appendage occlusion
Introduction- Atrial fibrillation affects greater than 2 million patients in Europe alone
- The lifetime incidence is 1:4 and it increases with age
Medical therapy
- While symptomatic management focuses on rate and/or rhythm control, prevention of complications focuses on stroke prevention
- Cerebrovascular thromboembolic events are the most feared complication of atrial fibrillation, and the risk of stroke can be individualized
- The CHADS2 and CHA2DS2VASc are the two most commonly used risk models
- Coumadin is the cornerstone of thromboembolic event prevention in atrial fibrillation, although non-vitamin K oral anticoagulant medications, such as dabigatran, rivaroxaban, apixaban and edoxaban may have similar efficacy and improved safety profiles
- For patients with CHA2DS2VASc scores of 0, either aspirin or no therapy is indicated. Scores of 1 or greater warrant oral anticoagulation.
Mechanical therapy
- The great majority of thromboembolic events in patients with atrial fibrillation arise from thrombus in the left atrial appendage
- Occlusion of the left atrial appendage may significantly reduce the risk of events, particularly in patients in whom anti-coagulation is contraindicated
- Surgical means of left atrial appendage exclusion have been evaluated with mixed results, particularly owing to incomplete closure and residual flow into and out of the appendage
- Percutaneous techniques are emerging as an effective means of LAA occlusion.
- Currently approved devices for LAA occlusion include Watchman, Amplatzer Amulet, Wavecrest, Cardia and L’Ambre.
General technical considerations
- Fluoroscopic and TEE guidance are imperative for successful procedure
- Location of transeptal puncture may vary by device shape and ensures coaxial alignment, potentially maximizing efficacy and minimizing complications
- LAA measurements taken by TEE and fluoroscopy with RAO caudal often providing the largest LAA dimensions
- A pigtail catheter with a soft wire is advanced past the transeptal delivery sheath to facilitate safe LAA engagement.
Watchman
- Available sizes: 21-33 mm in 3 mm increments with sizing aimed to achieve 8-20% compression of the device at the inferior ridge of the LAA.
- Minimum LAA length is 19 mm as each device is of similar length
- Treatable LAA width 17-31 mm.
Amplatzer® Amulet
- Transeptal puncture ideally anterior and inferior within fossa to ensure coaxial device alignment.
- Device sizes available are 16-34 mm in 2 mm increments with sizing 10-20% larger than landing zone by TEE.
- Minimum LAA length is 10 mm.
- Treatable LAA width 11-31 mm.
Lariat
- Suture mediated via epicardial access.
- Maximum LAA diameter is 40 mm.
- Maximum LAA height is 20 mm.
- Maximum LAA length is 70 mm.
- Anatomic exclusions include posterior or superior LAA rotation behind pulmonary trunk.
- Prior cardiac surgery is clinical exclusion.
Coarctation of the aorta
Surgical repair of coarctation- Surgical repair of coarctation is indicated in infants and young children in whom results are excellent
- Patch aortoplasty is associated with post-operative aneurysm formation
- Re-coarctation can complicate both subclavian flap repair and end-to-end anastomosis
- Hypertension remains a significant long-term problem
Balloon angioplasty for coarctation
- Is indicated in re-coarctation in infants and young children
- Provides excellent acute relief of obstruction in native and recurrent coarctation
- Is associated with a high rate of re-coarctation, particularly in native lesions in neonates and infants
- Is associated with aneurysm formation
Stenting of coarctation
- Stenting of coarctation is indicated in both native and re-coarctation in older children, adolescents and adults
- Biodegradable scaffolds, growth stents or dilatable stents are now the focus of research in neonates and small children
- Careful planning prior to catheterisation is essential
- The main complications are stent migration and aneurysm formation
- Follow-up must include imaging such as CT or MRI
Hypertension following surgical repair or percutaneous management of coarctation
- Is related to a pervasive vasculopathy characterised by arterial stiffness, independent of any residual aortic obstruction
- Is frequently seen many years after repair or intervention
- Is an important determinant of long-term morbidity and mortality
- May require 24-hour ambulatory measurement and exercise-stress assessment for detection
- Necessitates an assessment of the need for further intervention, which frequently reduces the requirement for anti-hypertensive medication
Interventions for congenital and acquired pulmonary vein stenosis
Pulmonary vein stenosis- PVS is a rare condition and not infrequently associated with other cardiac malformations and prematurity [1, 2]
- PVS is a progressive illness and unless good surgical relief can be obtained early in the course of the disease the course becomes recalcitrant to further therapeutic intervention with long-term results being generally disappointing [3]
- In this context interventional procedures must be regarded as palliative, with a primary objective of symptomatic improvement [4]
Interventional management
- Multiple procedures may be necessary and angioplasty is the initial technique of choice [1]
- In the presence of a fixed lesion, despite high inflation pressures of a non-compliant angioplasty balloon, a cutting balloon might be considered [5, 6]
- Where there is significant recoil of a lesion and the clinical circumstances demand a good result, a stent may be placed [7]
Carotid artery stenting
When to intervene in patients with severe carotid disease- The sole incentive for the treatment of carotid artery stenosis is stroke prevention
- In symptomatic severe carotid disease, updated guidelines provide clear recommendations for individual treatment strategies
- In asymptomatic lesions, the stroke risk associated with any type of prophylactic intervention should not exceed the risk inherent in the natural course of carotid atherosclerosis: 1%-3% per year
- This low risk for clinically asymptomatic carotid disease may become significantly higher in specific subsets (8% to 14% per year)
- For CAS, the experience of hospitals and physicians correlates with patient outcomes
Towards a safer carotid stenting
- Recognise in advance all the clinical and anatomical situations which can expose the patient to higher risk for carotid stenting
- The way to access the common carotid artery safely, EPD selection and management, stent selection and implantation are key elements for reducing procedural complications
Cerebral protection during CAS
- Filter protection, advantages: very intuitive device, maintenance of cerebral perfusion
- Filter protection, disadvantages: pass lesion unprotected, need for a suitable landing zone in the ICA, unreliable vessel wall apposition, difficulty of negotiating tortuous anatomies and tight lesions
- Proximal protection, advantages: recommended in challenging anatomies (difficult to access ICAs due to very angulated ICA-CCA take-off, tortuous ICAs, lack of a suitable ICA landing zone)
- Proximal protection, disadvantages: 8-9 Fr introducer sheath compatibility (patient with peripheral diffuse disease), interruption of brain perfusion (intolerance to occlusion takes place in 3-8% of the cases)
- The more risky the plaques and the anatomies you are going to address, the more the use of proximal protection devices is indicated
Stent selection
- Stent scaffolding and conformability play a significant role not only for achieving good procedural results, but also for improving 30-day outcomes
- Stents may exert intrinsic anti-embolic properties
- For open-cell design, the greater the cell size, the higher the potential for plaque penetration and intra-strut prolapse
- The more risky the plaque and the bifurcation anatomy you are going to address, the more the use of high scaffolding and high conformable frames is indicated
Carotid stenting complications
- Carotid stenting is anything but a simple and complication-free procedure
- Interventionalists should be adequately prepared for recognising and managing procedure-related complications
Subclavian, brachiocephalic and vertebral interventions
When to intervene in patients with subclavian and brachiocephalic disease- Revascularisation is indicated only in symptomatic patients
- In patients with atherosclerotic lesions of brachiocephalic trunks, endovascular approach is indicated as first treatment strategy
- Revascularisation of an asymptomatic patient with severe stenosis of brachiocephalic trunks may be indicated only in case of former or future mammary-coronary bypass, or for monitoring blood pressure in bilateral upper limb occlusion
When to intervene in patients with extracranial vertebral artery disease
- In patients with symptomatic extracranial vertebral artery stenosis, endovascular treatment may be considered for lesions ≥50% in the case of recurrent ischaemic events despite optimal medical therapy
- The use of an EPD should be considered on a case-by-case approach after evaluation of anatomical challenges and global embolic risk
- Revascularisation of an asymptomatic vertebral artery stenosis is not indicated, irrespective of the degree of stenosis
Interventions in the reno-visceral circulation
Renal artery stenosis- Atherosclerosis is the most frequent aetiology of RAS (approximately 90%) with preferentially ostial location
- Stenting has become the therapy of choice with annual restenosis rates of about 10% with current devices
- Fibromuscular dysplasia, the second most frequent cause of RAS affecting mostly young female patients, is primarily treated with balloon angioplasty only
Clinical consequences and aim of renovascular intervention
- Clinical consequences of atherosclerotic RAS include deterioration of pre-existing essential hypertension, impairment of myocardial function (both diastolic and systolic), and, in the presence of bilateral RAS or RAS of a single functional kidney, renal insufficiency and flash pulmonary oedema
- Revascularisation of significant RAS might result in improved blood pressure control, reduction of left ventricular hypertrophy and stabilised renal function
Imaging modalities and renal artery stenosis
- The key to clinical success in endovascular treatment of RAS is the appropriate patient selection in terms of correctly identifying a haemodynamically relevant RAS
- Duplex ultrasound as a non-invasive modality is the most reliable functional diagnostic tool to detect severe RAS
- The measurement of pressure gradients at rest and after pharmacological stress with drugs such as adenosine and dopamine (FFR) is reserved as a preprocedural diagnostic technique in angiographically equivocal lesions
Arterial access for renovascular intervention
The femoral access for renal artery intervention is most frequently used. In variant take-off anatomies a brachial or even a radial access has to be used
Renal ostial intervention
For ostial lesions the appropriate angulated view of the C-arm is essential to identify correctly the most severe lesion area and the exact position of the take-off of the renal artery to guarantee a correct stent position
Renovascular intervention
- In atherosclerotic RAS the guiding catheter technique is the safest, fastest and most effective interventional technique
- The key to the clinical success of the intervention is avoiding distal embolisation by using dedicated techniques such as “no-touch techniques”
- The role of distal protection devices and the use of GPIIb/IIIa receptor antagonists is still uncertain
- Measurement of resting pressure gradients and hyperaemic pressure gradients and the renal frame count might be helpful in determining significance of an angiographically borderline RAS
- A stent system dedicated for ostial lesions flaring the proximal end of the stent to the aortic wall improves re-engagement of the stent in case of in-stent restenosis
- Considering the acceptable low restenosis rates of bare metal stents, the role of drug-eluting stents and covered stents is still uncertain, randomised controlled trials with these devices are still on-going
Renovascular intervention for fibromuscular dysplasia
Balloon angioplasty is still considered the treatment of choice for FMD of the renal arteries. However, suboptimal acute results and restenosis might be more frequent as reported in the literature. Thus, the use of focal force balloons such as the cutting balloon is under investigation in order to improve further the technical results of the endovascular treatment of renal FMD
Renovascular post-intervention management
- Careful documentation of the final interventional results after wire retrieval (‘’wire out shot’’) is essential for the detection of more distally located complications such as perforations or embolism
- Post-interventional drug therapy is adapted from coronary guidelines for bare metal stent deployment, recommending dual antiplatelet therapy for at least 4 weeks
- Pre-discharge diagnostic evaluation should consist of duplex ultrasound to confirm vessel patency, measurement of serum creatinine ideally earliest 48 hours after the procedure in order to detect deterioration of renal function as a result of embolism or contrast-induced nephropathy. Moreover, 24-hour ambulatory measurement of the blood pressure should be performed
- Outpatient follow-up procedures should be recommended 6 and 12 months after the procedure and annually thereafter
- About 80% of in-stent restenoses develop during the first 6 months following the intervention
Evidence base for renovascular intervention
- Recent randomised controlled trials suggest no benefit from stenting of RAS over medical therapy only. However, these trials had substantial limitations in study design and patient selection and cannot be applied to any patient presenting with RAS
- In patients with RAS of aetiology other than atherosclerosis, endovascular treatment is still the treatment of choice with a high probability of curing hypertension
- In selected patients with severe atherosclerotic RAS, clinical benefits have been demonstrated in terms of improved renal function, blood pressure control and regression of left ventricular hypertrophy
- Proper patient selection and safe interventional techniques are key issues for the clinical success of the endovascular treatment of RAS
Mesenteric vascular disease
- Whereas acute mesenteric ischaemia can be diagnosed relatively easily and is still a major indication for surgical repair, chronic mesenteric disease remains a diagnostic challenge. Even if there are typical clinical signs that should lead to the right diagnosis, this is frequently delayed due to a wide variety of more frequent differential diagnoses
- Atherosclerosis is the leading cause of the disease and at least 2 out of the 3 mesenteric arteries must be affected to result in clinical symptoms
Clinical manifestation of chronic mesenteric ischaemia
Depending on the collateral circulation and lesion location, CMI can mimic different kinds of gastric and enteric disorders. Typically, symptoms are related to food intake associated with unintended weight loss
Atherosclerotic mesenteric ischaemia
CMI of atherosclerotic origin is frequently associated with atherosclerosis in other vascular beds such as the coronary arteries. This results in an increased overall cardiovascular mortality as in patients suffering from atherosclerotic RAS. CMI can convert to acute mesenteric ischaemia in cases of acute local thrombosis
Imaging modalities and mesenteric artery disease
- Duplex ultrasound is the diagnostic measure of choice for detection of proximal occlusive mesenteric disease
- Additional three-dimensional diagnostic procedures such as MR- and CT-angiography facilitate the planning of an endovascular interventional procedure
- Intra-arterial angiography is no longer indicated as diagnostic tool
Revascularisation strategy in mesenteric disease
- Asymptomatic CMI has to be treated conservatively with focus on secondary prevention of atherosclerosis
- Endovascular stent-based angioplasty has widely replaced open surgical reconstruction in symptomatic patients due to less invasiveness and lower complication rates at the expense of higher restenosis rates even of stent placement compared to surgery in atherosclerotic disease
- Revascularisation of two affected vessels might result in more durable freedom from recurrent symptoms compared to a single vessel revascularisation
Vascular access for mesenteric intervention
For anatomical reasons access from the upper extremity is preferred for the endovascular treatment of CMI
Invasive angiographic imaging of the coeliac axis vessels
A strict lateral angulation (90 degree projection) of the C-arm is appropriate for a proper opacification of the origin of the coeliac trunk and the superior mesenteric artery
Mesenteric percutaneous intervention
- The guiding catheter technique is the preferred technique for mesenteric artery revascularisation
- Stenting is strongly recommended for atherosclerotic ostial lesions, whereas for lesions affecting the trunk balloon angioplasty might be sufficient
- A dedicated ostial stent device facilitates the proper stent positioning
Post-intervention management of mesenteric intervention
- Post-procedural angiography, including the peripheral branches to exclude wire-induced complications and distal embolisation, is mandatory using DSA technique
- Post-interventional medication consists of dual antiplatelet therapy for four weeks followed by ASS only for life in adaption of the coronary practice
- Follow-up is based on duplex ultrasound
Peripheral arterial occlusive disease
Epidemiology and clinical presentation of PAD- PAD is encountered in up to 20% of patients in primary care over the age of 65
- PAD risk factors include advanced age, male gender, cigarette smoking, diabetes mellitus, arterial hypertension, dyslipidaemia and hyperhomocysteinaemia
- Clinical presentation of PAD ranges from asymptomatic through to critical limb ischaemia
Diagnostic modalities
- Clinical examination
- Haemodynamic workup (oscillometry, ankle brachial index [ABI], great toe pressures)
- Imaging studies (duplex ultrasound, magnetic resonance or computed tomography angiography or intra-arterial angiography, sonographic quick-screen for abdominal aortic aneurysms)
Conservative treatment of PAD patients
- Smoking cessation
- Control of diabetes mellitus (HbA1c values <7%)
- Control of dyslipidaemia (LDL target value <70 mg/dl)
- Control of arterial hypertension (target values <140/90 mmHg or <130/80 mmHg in the presence of diabetes mellitus or renal insufficiency)
- Antiplatelet therapy
- Vasoactive drugs (Cilostazol or Naftidrofuryl) if exercise training or arterial revascularisation cannot be accomplished
- Intravenous application of prostanoids in CLI patients with revascularisation failures or whose only alternative is major amputation
- Medical pain control in CLI patients
- Local wound care
- Exercise training
Indication for revascularisation and treatment strategies
- Arterial revascularisation is optional in claudicants and absolutely indicated in CLI patients without specific contraindications
- Endovascular and open surgical techniques are complementary and both have their pros and cons
- The decision as to which revascularisation method to apply should be tailored to the specific patient’s needs and based on multidisciplinary consensus
- Within this framework, endovascular revascularisation is increasingly established as first-line treatment concept for most claudicants and CLI patients alike
Interventions for varicose veins
Introduction- Clinical characteristics of chronic venous disease are telangiectasias, reticular veins, varicose veins, edema, eczema, hyperpigmentation, lipodermatosclerosis, white atrophy, corona phlebectatica and venous ulcers
- Varicose veins are manifestations of chronic venous disease, which may lead to serious complications
- Venous ulcers, which are the end-stage of chronic venous disease, have a prevalence of 1-2% in people older than 65 years
- Primary varicose veins have an anomaly of the vein wall matrix or the cusps of the valves
- Secondary varicose veins are usually due to deep vein thrombosis
History
- Compression therapy has been used since ancient times and still plays an important role in phlebology
- Ligation and stripping has been the standard of treatment for the saphenous veins for more than 100 years
- Endovenous (thermal) ablation techniques under local anesthesia are nowadays most frequently used
- The newest concept concerns the treatment of saphenous tributaries, which may lead to the abolition of saphenous reflux
Ultrasound examination and anatomy
- Ultrasound examination is the gold standard in assessing varicose veins
- Ultrasound examination should comprehend assessment of the superficial and deep venous system and perforating veins
- Knowledge of the venous anatomy and understanding the venous haemodynamics is essential for choosing the appropriate treatment
Treatment modalities
- Endovenous thermal treatments can be performed in an outpatient setting using tumescent anaesthesia
- Linear varicose veins are best treated by endovenous thermal ablation
- Tortuous recurrences are best treated by phlebectomies or UGFS
Procedures and their mechanism of action
- Endovenous treatment is always performed using ultrasound examination
- The sclerosant that is used with UGFS leads to phlebitis of the varicose vein
- EVLA and RFA work by thermal destruction of the varicose vein
- Cyanoacrylate seals the vein by an inflammatory vein wall reaction
Efficacy
- Sclerotherapy with foam is more effective than sclerotherapy with liquid sclerosant
- Endovenous (thermal) ablation therapies are the treatment options with the highest success rate
Complications
- Hyperpigmentation is the most common side effect of sclerotherapy
- The risk of DVT with endovenous procedures is low (<1%)
- Device-related complications of endovenous treatments are rare, but serious
Closure of arteriovenous fistulae and malformations
Coronary fistulae- The most common feeding artery is the right coronary (52%) followed by the left anterior descending (30%) and the circumflex (18%)
- The most common entry site is the right ventricle followed by the right atrium, coronary sinus, left ventricle and pulmonary artery
- Most fistulae are asymptomatic and are diagnosed in childhood due to a murmur. Some discovered in childhood may close spontaneously
- Symptoms are high output failure, ischaemia (related to a steal phenomenon), thrombotic events, ventricular arrhythmias and infectious endocarditis
- Rupture, though it can occur, is rare
- Treatment of asymptomatic fistulae is controversial. Symptomatic fistulae or those that progressively increase in size or are associated with a high shunt volume should be closed
- The treatment of choice is coil or vascular plug embolisation
- Small coronary AV fistulae related to myocardial biopsies should be managed conservatively
Non-coronary cardiac fistulae
- These include fistulae related to rupture of a sinus of Valsalva aneurysm (usually of the right coronary sinus) into a right heart chamber
- Traditionally surgery has been the treatment of choice
- Percutaneous repair has been demonstrated (e.g., with an AMPLATZER® occlude)
- Similarly closure of ventricular pseudoaneurysms with ASD or VSD occluders has been described
Pulmonary AV fistulae
- Pulmonary AV fistulae are a typically a manifestation of (autosomal dominant) hereditary haemorrhagic telangiectasia (HHT)
- The risk of AV malformations in patients with HHT is higher in the presence of the endoglin mutation
- Symptoms and signs include haemoptysis, paradoxical embolism, right heart failure or hypoxemia. A bruit by auscultation is heard only in the minority of patients
- More commonly than not fistulae are multiple (average: three)
- Contrast echocardiography is an excellent screening test (sensitivity >90%)
- Fistula closure is recommended even for asymptomatic fistulae fed by an artery of >3 mm diameter to prevent embolic events. Most would recommend staged closure when more than one fistula is present
- Contraindications to fistula closure are: active pulmonary infection and greater than moderate pulmonary hypertension
- The treatment modality of choice is coil or vascular plug embolisation
- Potential complications unique to this procedure are: pleuritic chest pain or pleural effusion (10% to 35%) and pulmonary infarction with subsequent infection
- Recurrence (up to 17%) is not uncommon. Follow-up contrast echo or chest CT is therefore recommended
Renal arteriovenous fistulae
- Renal AV fistulae are rare. Most are acquired (70%) (iatrogenic or trauma)
- Symptoms and signs include haematuria, hypertension (in 40% of patients) and high output failure. An abdominal bruit is common
- Acquired fistulae frequently resolve spontaneously. Most asymptomatic fistulae do not need to be treated
- The treatment method of choice is percutaneous coil or vascular plug delivery depending on the fistula size
Hepatic AV fistulae
- The most common feeding artery is the hepatic artery (60%)
- Clinical features include oesophageal varices, ascites, splenomegaly, intestinal or pancreatic ischemia, haemobilia or gastrointestinal haemorrhage. Right heart failure and pulmonary hypertension are uncommon
- Imaging modalities are ultrasound, MRI or contrast CT
- Small asymptomatic fistulae can be managed conservatively with non-invasive imaging follow-up
- Treatment of symptomatic fistulae or asymptomatic fistulae causing portal hypertension is recommended
- Asymptomatic extrahepatic arterioportal fistulae should be considered for closure
- Percutaneous treatment is the first choice in anatomically suited fistulae. Depending on the size and location, coils or vascular plugs can be considered
- Potential complications are liver failure (from liver infarction), portal vein thrombosis, biliary fistulae, stricture formation of stroke
- Accidental hepatic artery embolisation usually does not have any clinical consequences except in a patient with compromised liver function at baseline
Arteriovenous fistulae as a result of percutaneous coronary or peripheral interventional procedures
- The incidence of AV fistulae after femoral artery catheterisation varies depending on the diagnostic modality: 1% with clinical auscultation and 3% with systematic ultrasound screening
- Risk factors are female gender, hypertension, left femoral (versus) right femoral access and anticoagulation
- Most fistulae are asymptomatic. Forty percent of fistulae close spontaneously. Most spontaneous closures occur within the first month of the procedure. Large fistulae and those patients on anticoagulation are less likely to close spontaneously
- Ultrasound is the imaging modality of choice. This demonstrates a continuous unidirectional velocity signal in the fistula tract
- Ultrasound compression frequently fails to obliterate the fistula. Symptomatic fistulae, particularly those which cause right heart failure should be considered for closure
- If the landing zone permits (enough distance of the fistula tract from the femoral bifurcation), a covered stent would be an option. Rarely, the fistulous tract is small and long enough to allow coil embolisation
Imaging
- The imaging modalities used to identify and characterise an AV fistula are ultrasonography-imaging, CT-imaging or MRI imaging
- Typical findings on ultrasound are a low resistance flow pattern in the feeding artery proximal to the fistula and
- Typical findings on CT or MRI imaging are venous enhancement in the arterial phase
Coils, vascular plugs and gel foam
- Coil sizing is paramount to the success of coil embolisation. The non-constrained diameter should be slightly larger than the feeding vessel diameter
- Controlled release coils allow easy retrieval prior to deployment. Hydrophilic catheters for coil delivery are useful
- Not all coils are MRI compatible
- Vascular plugs are used for large feeding vessels. A plug diameter 30% larger than the diameter of the feeding vessel is recommended
- Some later generation plugs can be delivered via 4 Fr or 5 Fr catheters
Alcohol septal ablation for hypertrophic obstructive cardiomyopathy
Indication for alcohol septal ablationCLINICAL INDICATION
- Symptomatic patients
- Drug-refractory or severe side effects of drugs
- Functional class III and IV or functional class II with objective exercise limitations
- Recurrent exercise-induced syncopes - Failure of prior myectomy or pacemaker
- Comorbidity-related increased surgical risk
- Intracavitary gradient >30 mmHg at rest and/or
- Provocable gradient >50 mmHg
- Valsalva manoeuvre
- Physiologic stress test (Echo)
- Post extrasystole - No dobutamine-induced gradients
- Echocardiography
- Subaortic, SAM – associated gradient
- Mid-cavitary gradient
- Exclusion of intrinsic mitral valve apparatus disorders - Coronary angiography
- Suitable septal branch
Technique of alcohol septal ablation
- 2 arterial catheters for simultaneous pressure recording
- Temporary pacemaker
- Coronary angiography with identification of target vessel
- RAO and LAO cranial - Wiring of estimated septal branch
- Primarily the use of soft tip wires - Use of short over-the-wire balloon
- Avoid LAD ballooning
- Exclusion of leakage - Myocardial contrast echo
- Stepwise slow (1 ml/minute) alcohol injection
- 1 ml alcohol/1 cm septal thickness - Balloon deflation and removal
- 10 minutes after final alcohol injection
- Monitoring at the CCU for 48 hours
Results in alcohol septal ablation
- Haemodynamic results
- >50% gradient reduction in >90% of patients
- Ongoing gradient reduction during follow-up
- Reduction of pulmonary artery pressure - Echocardiographic results
- Septal thinning
- Posterior wall thickness reduction
- Mitral regurgitation reduction
- Left atrial size reduction - Exercise test
- Increase of exercise capacity
- Increase of peak oxygen consumption - Clinical results
- Improvement of functional class
- Symptomatic relief - Reduction of syncopal episodes
Complications of alcohol septal ablation
- Hospital mortality
- Complete heart block
- Remote acute infarction
- Alcohol leakage retrogradely to LAD
- Alcohol misplacement
- Inadvertent echo-contrast misplacement
- Inadvertent intraseptal collateralization
- LMS or LAD dissection
- Emergency surgery
- Coronary damage
- Acute mitral regurgitation
- Pericardial tamponade - Puncture site complications
- Haematoma
- Pseudoaneurysm
- AV-fistula
Alternative techniques to alcohol septal ablation for hypertrophic obstructive cardiomyopathy
Principles and methods of non-alcohol septal embolisation- Coil embolisation avoids direct toxicity of alcohol on the conductive tissue
- Coils are delivered inside the septal perforator artery through a microcatheter. Usually 2 to 3 coils/artery are needed
- Small polyvinyl alcohol foam particles adhere to the vessel wall causing thrombosis and inflammation
- Injection of n-butyl cyanoacrylate (n-BCA) into an epicardial artery results in a well demarcated homogeneous infarct
- Embolisation of glue material into the left anterior descending artery can happen during microcatheter retrieval
Results for non-alcohol septal techniques
- High procedural success rates (90%-100%) were reported for coil embolisation, PVA foam particle injection and glue septal ablation
- Coil embolisation results in a significant and sustained improvement in symptoms and reduction in LVOT gradient in 90% and 75% of cases, respectively
- Cardiac magnetic resonance imaging and creatine kinase (CK) rise suggest a smaller infarct size with coil embolisation than with ASA
- GSA results in the smallest infarct size among the three alternative techniques as assessed by the CK rise
Complications
- Very low number of complete heart block requiring permanent pacemaker implantation was reported with coil embolisation or polyvinyl alcohol foam particle injection or glue septal ablation
- Transient AV blocks were seen in 17% of patients treated with PVA foam particle injection
- Embolising glue material into the LAD artery and microcatheter retention are two possible complications during GSA
- In the dog model, n-BCA injection results in a chronic granulomatous inflammation of the vessel wall, the clinical significance of which remains unknown
Direct endocavitary ablation techniques
- Endocavitary radio-frequency ablation through the LV or RV cavity of a 2 cm2 of IVS is considered enough to produce a defect comparable to that with ASA.
- Mapping of the His bundle during ERASH is essential to prevent CHB
- ERASH results in a lower LVOT gradient reduction as compared to ASA
- High rate of CHB (21%) requiring permanent pacemaker implantation
Concept, techniques and clinical effectiveness of renal nerve ablation in hypertension
Hypertension and cardiovascular diseaseHigh blood pressure is highly prevalent in the overall population and represents a major risk factor for cardiovascular diseases:
- myocardial infarction
- peripheral artery disease
- stroke
- dementia
- chronic renal failure
Secondary hypertension
Determining possible secondary causes of hypertension is an important part in diagnosing patients with elevated blood pressure. The following (including less common causes of hypertension) should always be excluded in severe hypertension, resistant hypertension or those aged <40 before starting or continuing long-term conventional pharmacological treatment:
- renal parenchymal disease
- renovascular disease
- phaeochromocytoma
- primary aldosteronism (Conn’s syndrome)
- Cushing’s syndrome
- coarctation of the aorta
- thyroid dysfunction (hypo or hyperthyroidism)
- primary hyperparathyroidism
- acromegaly
- obstructive sleep apnoea
- drug/toxin-induced
- monogenic renal tubular syndromes
- pre-eclampsia
The sympathetic nervous system
- Hyperactivity of the sympathetic nervous system is one of the pivotal ‘players’ in the pathogenesis of arterial hypertension
- The sympathetic nerve fibres are distributed ubiquitously within the heart, the blood vessels, the kidney, and major peripheral baroreceptor sites, a finding that suggests a direct effect on:
- fluid balance
- cardiac output
- peripheral vascular resistance
Renal nerves and hypertension
- The kidneys play a key role in long-term pressure regulation through efferent and afferent nerves
- The surgical and pharmacological blockade of the renal nerves were found to be effective in reducing blood pressure, but were also associated with an increase in serious side effects
Techniques of myocardial stem cell delivery
Cardiac stem cell therapy- Cell therapy is an emerging therapy used as an adjunctive treatment after STEMI, chronic myocardial ischaemia and in patients with ischaemic or non-ischaemic congestive heart failure
- Factors affecting the final biological and functional therapeutic outcome are multiple and relate to patient-specific variables, such as functionality of autologous cells, choice of cell type or patient-independent parameters, such as stem cell processing
- Low rates of cell retention and variable biodistribution are common features of current clinical experience which will require attention in the future clinical adoption of cellular strategies
Coronary cell delivery
- Coronary cell transfer using the “stop-flow” method is the preferred method of delivery early after STEMI
- The optimal time window for coronary delivery depends on the balance between multiple putative and detrimental factors governing the infarction healing which appears to be most favourable between day 3 and 7 after the infarction
- Over-the-wire balloon catheter are the most widely used device for cell transfer
- New devices such as an infusion catheter allowing the periadventitial cell delivery may offer higher retention rates. Early experience suggest a favourable safety profile of the device
- The clinical efficacy of retrograde coronary venous infusion remains undetermined
Direct intramyocardial cell delivery
- Percutaneous endoventricular delivery, as a standalone procedure, can be used in ischaemic heart failure under fluoroscopic or electromechanical guidance
- Three injection catheters have been used so far in clinical trials of cell delivery: the Helix™ infusion catheter (BioCardia Inc., San Francisco, CA, USA) with a helical needle and MyoCath™ (Bioheart Inc.) and MyoStar™ (Biologics Delivery Systems) with a straight needle
- The injection strategy and target areas should be well planned in advance using the available clinical information
- Injections should be performed by a dedicated team after prior training. The needle extension must be performed swiftly after having established stable and perpendicular contact with the vessel wall as documented under fluoroscopic or electromechanical guidance. The injection of the biologics should be performed slowly to allow for the fluid absorption by the myocardium
Future development of cell delivery techniques
- Strategies to improve cell delivery and retention include better understanding and exploration of the myocardial niche-cell and device-niche interaction
- Tissue priming, or cell priming including the use of cell scaffolds, are under testing to improve cell retention and survival
- Mathematical modelling, hand in hand with experimental in vitro and in vivo testing, is a sound platform to validate various needle designs to improve cell retention
Pulmonary embolism and pulmonary hypertension
Incidence of thromboembolic disease and pulmonary arterial hypertensio- Yearly incidence of pulmonary embolism 69/100,000 [1]
- Yearly incidence of pulmonary arterial hypertension 2.4-15/1,000,000 [2]
- Yearly incidence of chronic thromboembolic pulmonary hypertension 5/1,000,000 [3]
The Heart team
Specialist involvement in the Heart TeamCoronary Heart Team should include at least:
- Surgeon
- Interventional cardiologist
- Primary non-invasive cardiologist
- Surgeon
- Interventional cardiologist
- Primary non-invasive cardiologist
- Image specialist
- Anaesthesiologist
Risk scores
- STS score for risk estimate of short-term operative mortality based on clinical factors
- EuroSCORE for risk estimate of short-term operative mortality based on clinical factors
- SYNTAX score for mid- and long-term coronary lesion complexity based on angiographic factors
- SYNTAX II score for combined clinical and angiographic long-term risk estimation
Tasks of the local coronary Heart Team
- Benchmarking decision-making
- Mortality and morbidity conferences
- Develop local institutional protocols for ad hoc PCI
- Develop local institutional protocols, based on international guidelines, on cases that require discussion to avoid systematic discussion of all diagnostic coronary angiograms
Conclusions
- For coronary artery disease and valvular heart disease, the Heart Team should be used for patient evaluation
- Several risk scores can be used to guide the Heart Team during the decision-making process
- The Heart Team is a IC indication in the current guidelines on myocardial revascularisation
- Patients with severe aortic stenosis should be discussed in a Heart Team according to the latest European guidelines on valvular heart disease
- Patients with severe mitral regurgitation in whom a percutaneous treatment strategy is considered should be subjected to a Heart Team discussion
Ethics in cardiovascular interventions
Ethics represents philosophical inquiry into the morality of rights and wrongs of human actions. Three major schools of ethics are teleology (consequentialism), deontology and virtue ethics. Medical ethics which relies largely on deontology also includes, depending on context, teleological and virtue ethical views. Doctors’ professionalism depends on understanding and attending to the principle maxims of ethics in daily clinical practice; preserving patient safety and well-being is the first of the promises to keep.
Medical ethics primarily reflecting the tenets of deontology follows the maxims of the established rules of normative ethics. In the Four Principles approach (Autonomy, Beneficience, Non-maleficience, Justice) the basic ethical obligations of doctors towards their patients have been summarized. While ethics is far more inclusive than the Four Principles approach, it represents a useful point of departure and commentary. Medical ethics underwrites doctor-patient relationships, based on fairness and mutual trust, formalized and legalized by thorough patients’ education and with signed written Informed Consent.
Medical law provides a legal framework for medical practice. Medical ethics defines the ideals for the conduct of medical professionals, emphasizing the ethical foundation of doctor-patient relationships based on mutual trust between two rational human beings.
Knowledge of legal aspects of patients’ education and consent as well as a thorough understanding of basic legal principles should complement the cognitive and other competencies of operators.
The practice of ethics in Interventional Cardiovascular Medicine is highly dependent on ethical integrity of operators. While the general virtues expected from all medical professionals also apply, operators, due to their exposed status, need to acquire a number of ICM specific professional virtues. The practice of virtues assures ethical integrity and long-term capacity in a highly competitive and demanding profession.
The cardiac catheterisation laboratory environment
Diagnostic functions of a cardiac catheter laboratory- Right heart catheterisation and angiography
- Right and left heart catheterisation and angiography
- Left heart catheterisation and angiography
- Coronary angiography
- Myocardial biopsy
- Pericardiocentesis
Requirements for a hybrid (valvular) catheter laboratory
Room
- Large size, ventilation/gases/suction, proximity to OR/ICU
- Ability to adjust range for soft tissue imaging
- Ceiling mountedequipment
- Rotational angiography capability
- Digital subtraction angiographic capability
Adjuctive imaging to aid:
- Pre-procedure planning
- Procedure execution
- CT guided procedures
- Registration with CT
- Imaging workstation and in-room monitors
- Navigations systems and robotics
- Supplies
- Toolbox for complications
- Haemodynamic monitoring
- Heart-lung bypass / anaesthetic equipment
Future perspectives
- Minimal invasiveness is the future
- Patient safety and efficiency will be the leading factors
- A more general specialist treating the cardiovascular patient will emerge who has to have a profound knowledge of future imaging
Future technological innovations
- Tissue characterisation will be performed in the near future allowing focused treatment
- We are on the threshold of 3D imaging without the use of x-ray and contrast
- Remote or robot surgery seems useful
Administration and data collection
Key fields for a procedure report- Patient demographics
- Clinical features
- Indication for procedure
- Procedural details
- Hospital identifier and operating team details
- Adverse events, complications, and patient experience
- Post-procedural and discharge plan
Clinical governance
- Education and training
- Research and development
- Openness with respect for confidentiality
- Risk management
- Clinical audit
Clinical audit domains
- Structure
- Appropriateness
- Process
- Outcome
Registry studies and post-marketing surveillance
Clinical quality registry- Provides an opportunity to systematically collect all clinical data about a certain diagnosis or medical procedure in order to describe and improve the quality of care
- Needs to have consecutive enrolment and ideally include all patients within a region
- Requires management and political support to ensure uptake and adequate resources
- Users must be trained and motivated professionals
- All levels of relevant healthcare providers must be engaged
- Stable and long-term financial support
Observational studies
- Drawn from large-scale registries, observational studies are complementary to prospective randomised trials
- Despite appropriate statistical adjustments there are always confounders that cannot be completely compensated
- It is thus important to be cautious in the interpretation of observational studies comparing outcomes between different treatment alternatives and always consider the results as non-definitive and hypothesis generating
Collection of outcome variables
- Crucially important for the evaluation of quality of healthcare
- Must be systematic to ensure complete patient capture
- Must cover as large a geographical region as possible
- Must be linked to national mortality registers
- Total mortality, both short and long term, is the most reliable hard endpoint
The randomised clinical registry trial
- Large-scale RCTs are expensive and logistically challenging to undertake
- In RCTs important clinical questions are frequently not addressed due to commercially driven and economic imperatives
- Randomising patients into a clinical quality registry combines the features of a prospective randomised trial with a large-scale clinical registry
- Unselected enrolment is a key strength of this form of study
Clinical trial design
Randomised controlled clinical trials- A well-conducted and analysed randomised controlled clinical trial is the most reliable scientific method for conducting medical research and provides the highest level of evidence
- A randomised controlled trial should only be conducted where clinical equipoise exists
- In a well-designed and conducted RCT all patient covariates, measured and unmeasured, are expected to be balanced between the two groups. Confounding is not a threat to the internal validity of a properly conducted RCT, and the observed treatment difference is an unbiased estimate of the true treatment difference
Observational studies
- Well-conducted observational studies can provide a more realistic assessment of the real-world outcomes of therapies, as compared with traditional but more restrictive RCTs
- A variety of statistical techniques (such as multivariable regression analysis, matching or stratification and propensity score methods) may be used in an attempt to correct for known and measured confounders and increase the internal validity of observational studies
Composite endpoints
- Composite endpoints (CEP) are common in cardiovascular trials. CEPs allow for a smaller sample size in the trial (for a given power) as a result of the increased event rate and deal with the “multiple testing” problem by combining multiple single endpoints
- All components of a CEP are considered statistically equivalent in the analysis, irrespective of their clinical importance
Subgroup analyses
Subgroup analyses are frequently performed in order to examine whether treatment differences appear consistent across all types of patients or vary according to subgroups. However, to avoid issues with multiple testing, it is important that only a limited number of pre-specified subgroup analyses be performed with cautious interpretation of findings
Intention-to-treat analysis
- An intention-to-treat analysis includes an analysis of all eligible patients (based on how they were initially randomised) regardless of their compliance with the therapy and follow-up
- A per-protocol or “as-treated” analysis includes all patients who completed the full course of assigned treatment
- An intention-to-treat analysis is the preferred form of analysis in most trials as it preserves the underlying randomisation process. It is usually the conservative form of analysis in the common superiority trial design setting. A per-protocol analysis will usually yield a higher effect estimate of the treatment effect in this setting
Quality of life assessment
QoL instruments- Qol questionnaires reflect the patient’s perspective
- they are validated measurements that demonstrate high reproducibilty
- QoL is an independent predictor for mortality and hospitalisation
- these measurements may provide additional information on treatment effects
- QoL measurements can contribute to the decision-making process (regarding choice of therapy)
- QoL questionnaires may facilitate communication between patient and physician
Risk-benefit analysis
Measures of health outcomeEvaluating benefits from medical procedures
- Disease-specific measures of health outcomes
-more sensitive to improvements in aspects of health which may be most likely to be affected by the proposed intervention - Generic measures of health outcomes
-broader spectrum, more relevant for policy decisions
Revascularisation and quality of life
Multiple studies have demonstrated improvements in QoL from pre-procedure to post-procedure for both PCI and CABG, when compared to medical treatment
- PCI clearly improves the QoL immediately following the revascularisation procedure
- CABG has less risk of repeat revascularisation but a higher comorbidity in the short term compared to PCI
- Given the improvements in outcomes from PCI over time (e.g., introduction of BMS and DES), reassessments of the benefits and risks from PCI versus CABG would be warranted
New methods in risk/benefit analysis
- Risk-benefit modelling can be used to demonstrate the trade-off that physicians and patients face in choosing between the deferred benefits of reduced rates of repeat revascularisation from CABG versus delayed relief from pain or improvement in HRQL
- This is important, from the patient’s perspective, in order to translate the risk and benefit deriving from different revascularisation procedures to something more tangible and easy to understand
- Risk-benefit acceptability curve (RBAC), analogous to the cost-effectiveness acceptability curves, provides estimates of the probability that a particular approach such as PCI is viewed by the patient as being risk-effective over different preference thresholds for the risk-benefit trade-offs identified
- In this way, the choice of PCI over CABG is a model of accepting greater long-term risk of additional revascularisation in exchange for reduced post-procedural morbidity, specifically pain and composite HRQL
Risk/benefit analysis in AS treatment
- TAVR approach provides a safe and efficient treatment for patients who are not suitable or are consideredat very high surgical risk of for SAVR.
- QoL assessment is important in this specific population at the time of decision between SAVR and TAVR
- Health status assessment showed that patients who underwent a TAVR present an earlier improvement in QoL, with similar results at 6 months and 1 year compared with SAVR.
Cost and cost-effectiveness
General scope and definitions- The uptake of revascularisation using PCI with or without stent has been rapid in developed countries
- There is a positive correlation between the rate of PCI and the wealth of a country
- The relationship between the rate of PCI and cardiac mortality is less straightforward
Confidence intervals for cost effectiveness
- Uncertainty of a variable within a population is conventionally estimated using statistical central limit theorem assuming a normal distribution and large sample size
- Economic data for populations tends to have small sample sizes and a skewed distribution
- Bootstrapping is an automated computer simulation method for the statistical inference of uncertainty (confidence intervals), and is suited to such complex datasets
- In bootstrap methodology rather than making assumptions about the underlying population the raw data itself is used. Random samples (replicates) of the same size are drawn from the original data at least 1,000 times to create empirically a distribution and hence the confidence intervals
Health technology assessment and interventional cardiology
- There is a well-accepted method to estimate the benefit of a new technology in relation to its cost: a cost-effectiveness ratio is the amount of money to be paid in order to obtain a gain in survival or a reduction in adverse events
- The World Health Organisation suggested in 2003 that the maximum amount to be paid be based on the per capita national GDP. An intervention that prolongs life by one year at a cost less than 1 x per capita GDP is inexpensive and a strategy that prolongs life by one year at a cost less than 3 to 5 x per capita GDP is expensive or even too expensive. In the UK the threshold usually mentioned is £30,000 or $50,000
Economic evaluation and interventional cardiology
- Revascularisation procedures are accepted to be cost effective in developed countries
- The cost effectiveness of systematically using DES instead of BMS is more controversial
Economic evaluation and TAVI
- TAVI is likely to be cost effective in patients not eligible for surgery
- Using TAVI instead of surgery is not cost effective
Interventional cardiology training
Invasive and interventional requirements for the general training of cardiologists (ESC Curriculum 2009)
Minimum requirements for interventional training according to the EAPCI curriculum

Essential terminology pertinent to medical training and revalidation

Consensus on definitions of clinical endpoints: percutaneous coronary and valvular intervention trials
The need for a consensus on endpoint definitions- Uniform, accurate and consistent event adjudication requires independent event adjudication based on trial specific or consensus definitions available in the field, providing outcome data sufficiently specific to be subjected to statistical analysis
- One of the most fundamental barriers to meaningful data aggregation is the use of different nomenclature and definitions of key descriptors and endpoints from one trial to another
Operational definition of a consensus endpoint
Consensus endpoint definitions should enable insight into the biological effect of the new device while providing sufficient knowledge about what really matters – how patients fare with regard to freedom from all-cause death, myocardial infarction, and repeat revascularisation procedures
The Academic Research Consortium
- An informal collaboration between academia, industry and regulators to standardise the definition of trial endpoints
- Currently consists of US (based at Harvard, Duke and the Cardiovascular Clinical Research Institutes), and European Investigators (based in Rotterdam, Bern and Paris), industry representatives and the US Food and Drug Administration
- First convened in 2006
- The ARC consensus endpoint definitions were initially conceived and work well for stable coronary disease patients with de novo lesions
Reporting mortality endpoints
- The ARC considers all-cause mortality the most unbiased method for reporting death
- ARC-2 proposes that the cardiac and vascular categories be merged into a single entity, cardiovascular, in order to be consistent with pharmacological studies
- Even when a distinction must be drawn between cardiac and non-cardiac mortality, the initial assumption is that a death is cardiovascular unless unequivocally demonstrated otherwise
- Clinical autopsies may help to establish the true cause of death and should be strongly recommended
Reporting acute myocardial infarction
- MI cannot be defined solely by biomarker elevations in the absence of new clinical signs (e.g., new pathological Q-wave) or symptoms consistent with myocardial ischaemia
- Acute ischaemic events occurring after 72 hours, and after the cardiac biomarkers have returned to normal, are considered spontaneous MIs and are defined in accordance with the universal MI guidelines
Reporting acute kidney injury for TAVI trials
- VARC favoured the RIFLE criteria for classifying AKI. VARC-2 favour the AKIN criteria
- An outer bound of 72 hours from the index procedure for diagnosing AKI was proposed by VARC. This has been extended to 7 days in VARC-2
- Any use of renal replacement therapies within 30 days of the index procedure should be reported
Consensus on definitions of clinical endpoints : carotid artery and supra-aortic trunk revascularisation trials
Internal carotid artery stenosis- Pre-intervention examination by a neurologist is mandatory
- Symptomatic carotid stenosis includes TIA, stroke or ischaemic ocular symptoms within the previous 6 months
- Clinically silent radiological lesions or symptoms>6 months are considered as asymptomatic
- A stenosis of 50% or greater is considered haemodynamically significant
- The NASCET criteria should be used to grade the stenosis
- Symptomatic patients with 50-99% stenosis and asymptomatic patients with 60-99% stenosis are potential candidates for revascularization
Vertebral artery stenosis
- Pre-intervention examination by a neurologist is mandatory
- Symptoms include: coma, cranial nerve palsy, diplopia, nystagmus, vertigo, dizziness, ataxia, visual field loss, hemiparesis or tetraparesis, pure hemisensory loss, and disorders of colour vision, face recognition or memory
- Only symptomatic patients with stenosis are candidates for revascularisation
Subclavian artery stenosis
- Symptoms include: Arm or brain embolic events, srm claudication, vertebral-subclavian steal syndrome, coronary-subclavian steal syndrome,, and subclavian steal syndrome in patients with a high-output dialysis arteriovenous fistula
- Symptomatic patients with stenosis or occlusion are potential candidates for revascularisation
Percutaneous closure of paravalvular leaks
The role of echocardiography during the procedure- Real time confirmation of defect crossing with guidewire or delivery sheath
- Ruling out interference of closure device with prosthetic valve function
- Accurately detect and quantify residual leaks
- Excellent tool for site specific puncture
The role of the CTA
- Best imaging tool for planning of the access and precise location of the defects
- CTA overlay facilitates defect crossing and can be used for the transapical puncture
- The CTA is not a real time and therefore has no value in device positioning
Selection of approach for mitral paravalvular leak closure
- Transseptal approach for leaks located at 6-11 o’clock
- Retrograde approach for leaks located at 10-1 o’clock
- Transapical approach for leaks located at 11-6 o’clock
Most common cause of failure
- Most common cause of failure is inability to cross the leak with guidewire or delivery catheter
Most common complications
- Access related:
- Bleeding
- Vessel dissection
- Cardiac perforation
- Arrhythmias - Device related:
- Acute/subacute device embolisation
- Interference with the prosthetic valve - Other:
- TIA/Stroke
- Worsening haemolysis
Endovascular treatment of acute ischemic stroke
IA pharmacological thrombolysis, key points- Used primarily as an adjunct treatment to aspiration or stent retriever thrombectomy
- Can be delivered via a small microcatheter positioned proximal to or inside the thrombus
- Contrast injection is performed through the microcatheter to ensure its satisfactory position and no perforation/active contrast extravasation
- rtPA is administered at rate of 1 mg/min, maximal dose of 10–20 mg. Frequently repeat angiography is performed to assess for revascularization
- Very gentle microwire manipulation can be used for adjunctive treatment (using a “J” tip is safer than a straight tip)
- Additional use of glycoprotein IIb/IIIa inhibitors is controversial
Aspiration thrombectomy, key points
- Requires a large-bore guide catheter (examples: Neuron MAX 088 from Penumbra, 6-French (F) Cook Shuttle long sheath from Cook Medical (Bloomington, Indiana, USA), or 8-9F balloon-guide catheter
- Choice of reperfusion catheter depends on the location of occlusion: use the JET family of aspiration catheters from Penumbra, Inc. or SOFIA 6F from MicroVention for ICA-terminus and proximal M1 MCA occlusions, JET D catheter from Penumbra, Inc. or SOFIA 5F from MicroVention for M2 MCA occlusions.
- In cases of tortuous anatomy, an aspiration catheter can be advanced over a 3MAX catheter and 0.014-0.018-inch microwire
- Continuous aspiration can be achieved manually using a 20-cc syringe or by connecting to the aspiration pump
Stent retriever thrombectomy, key points
- 0.021–0.027-inch microcatheters can be used to deliver most stentrievers
- The microcatheter is advanced over the microwire through the thrombus and microinjection is performed to ensure adequate position of the microcatheter
- The stent retriever is unsheathed under direct fluoroscopy, and the interventionist waits 3-5 minutes to allow the stent retriever struts to engage the clot
- If successful revascularization is not achieved, repeat thrombectomy attempts with the same device are recommended (typically 3 attempts are recommended, depending on the manufacturer). If still unsuccessful, consider changes the size or brand of the stent retriever.
- If using a balloon-guide catheter, inflating the balloon during the retrieval step might decrease the chance of inadvertent distal embolization
- For the combined stent retriever + aspiration thrombectomy approach, a large-bore guide (examples; Neuron MAX 088 from Penumbra, 6F Cook Shuttle long sheath from Cook Medical, 9F balloon-guide catheter from Stryker) that can accommodate an appropriately-sized aspiration catheter. The proximal end of the stent retriever is engaged within the tip of the aspiration catheter to facilitate capturing the clot.
Summary of the 2019 AHA/ASA update on endovascular management of acute stroke (adapted from Corrections [authors anonymous], [59])
- Strongest evidence supports mechanical thrombectomy for patients with ICA or MCA M1 occlusion and NIHSS and ASPECTS ≥6 in whom treatment can be initiated within 6 hours of stroke onset.
- In carefully selected patients, such as those with more distal occlusions, posterior circulation occlusion, and NIHSS <6 or ASPECTS <6, mechanical thrombectomy within 6 hours may be reasonable.
- In carefully selected patients within 6 to 24 hours of symptom onset, including wake-up strokes, mechanical thrombectomy is indicated in patients who meet DAWN and DEFUSE 3 eligibility criteria.
- Direct aspiration is noninferior to stent retriever use.
- The choice of anesthesia (conscious or general) can be individualized (previous recommendations favored conscious sedation over general).
Summary of the 2018 European Stroke Organisation (ESO) - European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on endovascular management of acute stroke (adapted from Turc et al. [60])
- There is high-quality evidence to recommend thrombectomy plus best medical management (including IV tPA) in patients with LVO AIS within 6 hours after symptom onset.
- There is a moderate quality of evidence to recommend thrombectomy plus best medical management in the 6-24 hour time window in patients meeting the eligibility criteria of published randomized trials.
Transcatheter tricuspid valve interventions
Anatomical challenges for transcatheter tricuspid valve therapies.- Large tricuspid annulus dimensions with a non-planar and elliptical shape
- Absence of calcifications
- RV morphology (trabeculae, muscle bands, thin apical wall)
- Proximity/contiguity of other structures (coronary sinus, AV node and bundle of His, venae cavae, right coronary artery)
- Angulation of the annulus in relation to the superior vena cava and inferior vena cava
Secondary prevention of atherosclerotic cardiovascular disease
Objectives of secondary prevention of CVD- No exposure to tobacco (not even second hand smoke)
- Diet: avoid dietary trans fats, reduce saturated fatty acids; increase wholegrain, vegetables, fruits, fish
- Physical activity: participation in a cardiac rehabilitation program followed by a medically prescribed aerobic exercise training program
- Body mass index: < 30 kg/m2; ideally between 20 and 25 kg/m2
- Waist Circumference: < 102 cm (men), < 88 cm (women); ideally < 94 cm (men), < 80 cm (women)
- Blood pressure: < 130/80 mmHg in patients aged < 70 yrs; < 140/80 mmHg in patients aged > 70 yrs or even lower if tolerated.
- LDL-C: < 1.4 mmol/L (55 mg/dL) and a reduction of at least 50% from the baseline level
- Diabetes: HbA1c < 7% (53 mmol/mol)
- Use of cardioprotective drugs as appropriate
Balloon pulmonary angioplasty
All patients who are ineligible for PEA, as well as those with residual or recurrent pulmonary hypertension after PEA, are candidates for BPA.Anticoagulants should be continued during BPA.
The success of BPA depends on the selection of the guiding catheter.
Avoiding overdilatation at the lesions in the initial session can reduce the risk of complications.
Indefinite anticoagulation therapy should be continued after BPA.
Using a guidewire with the smallest possible tip load is recommended.
Coughing with or without bloody sputum during BPA is a warning sign of pulmonary vessel injury.
All segmental pulmonary arteries and all types of lesion should be treated.
The interventional management of out-of-hospital cardiac arrest
Since the number of patients with out-of-hospital cardiac arrest (OHCA) admitted to hospitals increases and because it is well known that significant coronary artery disease may be present in more than 70%, interventional cardiologists are increasingly alerted for coronary angiography (CAG), percutaneous coronary intervention (PCI) and implantation of invasive hemodynamic support devices.
Clinical presentation of OHCA patients at hospital admission differs significantly in terms of hemodynamic stability, neurological status and likelihood for neurological recovery.
In the presence of ST-elevation myocardial infarction (STEMI) on the early post resuscitation electrocardiogram (ECG), an acute culprit lesion may be found in up to 90% of cases. Absence of STEMI does not exclude acute culprit lesions which may still be present in 25% to 58% of cases.
Many observational cohort trials demonstrated the feasibility, safety and possible survival benefit of immediate CAG in OHCA. Four randomized trials in a subgroup of “comatose” survivors of OHCA without STEMI did not show a survival benefit of an immediate compared to selective/delayed CAG/PCI strategy. There are no published or ongoing randomized trials on immediate CAG/PCI in “comatose” survivors of OHCA with STEMI.
Selection of patients for immediate CAG/PCI should be individualized to obtain the maximal benefit and avoid futility. Several factors including the cause of OHCA, pre arrest comorbidities, time delays during prehospital resuscitation, level of consciousness, post resuscitation ECG and hemodynamic status on admission should be analyzed on a per patient basis.
Invasive physiological assessment of coronary disease: non-hyperaemic indices (iFR)
Background and guideline recommendations for physiological assessment of intermediate stenoses- Physiology-based management of coronary artery stenosis has demonstrated improvement in outcomes as compared with angiographic guidance.
- Fractional flow reserve is a hyperaemic index that requires the use of adenosine.
- Instantaneous wave free ratio (iFR) is a non-hyperaemic index which evaluates the ratio of distal and aortic pressure during the wave-free period of diastole.
- Both FFR and iFR have a class IA recommendation for the assessment of the haemodynamic relevance of intermediate stenoses in clinical guidelines of revascularization.
Validation of iFR
- Values of iFR and FFR are significantly and closely correlated
- iFR has a good diagnostic accuracy to predict and FFR<0.80.
- iFR has been validated against myocardial perfusion scintigraphy and PET showing good diagnostic accuracy with values of area under the curve similar to those of FFR.
- CFR is more strongly correlated to iFR than to FFR.
Clinical trial data supporting the use of iFR
- The DEFINE-FLAIR was a prospective, multicentre, international, double blinded trial in which 2492 patients with intermediate severity coronary artery lesions were randomized 1:1 to undergo either iFR-guided or FFR-guided coronary revascularization
- The iFR SWEDEHEART was an open-label multicentre, registry based randomized clinical trial in which 2037 patients with intermediate coronary stenoses were randomized 1:1 to iFR or FFR guided revascularization.
- Both trials demonstrated that iFR was not inferior to FFR to guide revascularization with similar outcomes in both groups at 1 year
- In both studies there was a lower occurrence of symptoms during the procedure in the iFR group. The DEFINE-FLAIR trial demonstrated also a shorter procedural time with iFR.
- The pooled analysis of both trials demonstrated that a significantly higher proportion of patients were deferred in the iFR-guided than in the FFR guided strategy but with similar rates of 1 year MACE in the deferred population in both groups.
Discrepancies between FFR and iFR values
- Discrepancies between FFR and iFR can be explained by different aspects such as differences in hyperaemic flow and microvascular disfunction.
- These differences between resting and hyperaemic pressure derived indices are the result of a complex interaction of clinical, anatomical and physiological characteristics of the patient and lesion.
- However, discordance between FFR and iFR has not been associated with an increased risk of MACE in deferred patients.
iFR in multivessel disease
- iFR simplifies functional stenoses assessment in terms of time consumption, adverse side effects and costs, aspects especially relevant in the setting of MVD.
- The SYNTAX II trial have demonstrated the value of iFR to guide coronary revascularization in patients with MVD.
- A contemporary PCI approach including physiologic evaluation, second generation drug eluting stents and imaging optimization demonstrated improvement of outcomes at 1 year as compared with the PCI cohort of the SYNTAX I trial.
- In the SYNTAX II trial physiological guidance decreased the initial angiography-based 3.5 target lesions per patient to 2.6 lesions per patient, and PCI was deferred in 25% of the lesions.
iFR in non-infarct related arteries in acute coronary syndromes
- Some studies have shown benefit of non-IRA physiologic evaluation to reduce revascularizations at follow up. However, there are no studies comparing angiographic vs physiology-based management of the non-IRA in acute coronary syndromes.
- There is no clear evidence about when is the optimal time to perform the physiological assessment of the non-IRA in patients with ACS.
- iFR has a high negative predictive value in the evaluation of non-IRA in the setting of ACS. The increase in resting coronary flow in ACS could decrease the iFR values obtained in the acute setting.
- Data from randomized clinical trials suggests an excess of events at one-year follow up in patients with acute coronary syndromes in whom revascularization deferral of non-IRA was based on physiology as compared to patients with stable angina. This was more relevant for FFR than for iFR.
- The potential advantages of one of the indices (FFR or iFR) in the evaluation of non-culprit stenoses in patients with ACS deserves further research.
Physiological assessment of coronary artery disease in patients with aortic stenosis
- Pressure-wire-based assessment of coronary stenoses, with both FFR and iFR, is feasible and technically safe in patients with severe aortic stenosis
- Resting indices could potentially offer the advantage of avoiding adenosine and its hemodynamic adverse effects in this fragile population.
- The singular underlying pathophysiological framework of aortic stenosis requires caution in interpreting coronary invasive physiological measurements before aortic stenosis treatment
iFR in the presence of serial stenoses
- Fractional flow reserve was validated for isolated stenosis, and its real value for a given lesion can be masked by the presence of downstream serial stenoses
- iFR can be a better tool for the evaluation of serial stenosis given the more stable behaviour of resting flow across the range of stenosis severity as compared with hyperaemic flow.
- With a pullback of the pressure wire a resting pressure pullback trace can be created in which the hemodynamic significance of each individual stenosis can be quantified.
- In serial lesions, the expected iFR result after treatment of an individual stenosis can also be accurately calculated (virtual PCI)
- The co-registration of iFR pullback and angiography allows the use of physiology to determine the disease pattern (diffuse vs focal stenosis) and guide treatment.
The role of imaging in coronary chronic total occlusion intervention
- Cardiac Magnetic Resonance Imaging becomes the central role of evaluating myocardial viability, whereas, fusion imaging of SPECT and MSCCTA provides disease anatomy and location of ischemia, simultaneously.
- IVUS plays a crucial role in CTO-PCI, especially for, 1) identifying the ambiguous proximal cap and puncturing the intimal plaque, 2) locating the intima- subintimal deviation point and navigating a second wire into the distal intimal plaque, 3) resolving the difficulty in bilateral wire (re) entry in a retrograde approach.
- IVUS assisted CTO PCI could provide better long term MACE free period in order of 2-3 years or more, compared with angiography-alone guided PCI, which raises the future direction for a need for large scale randomized multi-center trial.
CT Coronary angiography for CTO PCI
- Evaluates anatomical features not evident on a conventional invasive coronary angiogram: proximal cap ambiguity, true length of occlusion, the amount and distribution of the calcified plaques, distal vessel size, degree of remodeling, presence of collaterals and entire vessel course.
- Through the CT-RECTOR score can grade complexity and predict the feasibility of guidewire crossing
- The imaging protocol should include 3D Volume Rendering (VR), Multiple Reconstruction (MPR) and Maximum Intensity Projection (MIP)
The high bleeding risk patient
High Bleeding Risk (HBR) patients are in many ways a “forgotten population” and have until recently been excluded from or under-represented in the majority of drug or device trials in patients undergoing PCI.
Given that HBR patients now constitute a growing proportion of PCI candidates, it has become urgent to create a standardised definition for this heterogeneous group, both for clinical trial design and for use at the bedside.
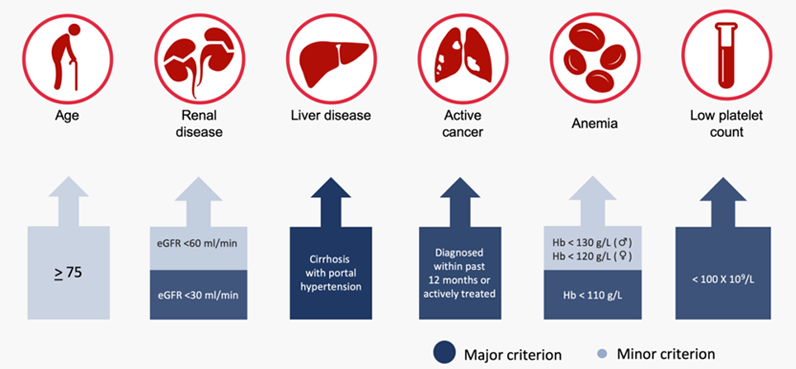
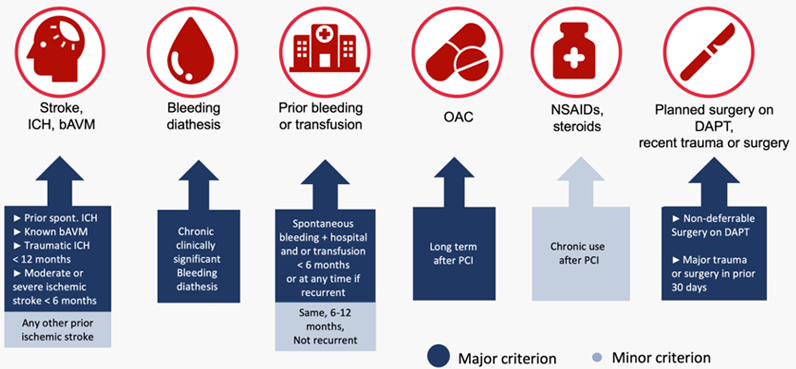
Computational non-invasive physiological assessment of coronary disease
- Reconstruction of geometrical data based on non-invasive or invasive coronary imaging
- Defining hemodynamic boundary conditions
- Computation of pressure data using computational fluid dynamics or fluid dynamics equations
- Naturely build-in co-registration between anatomy and physiology
- Possibility to associate plaque characteristics with functional evaluation
- Nitrates administration prior to image acquisition is mandatory
- No other hyperemic agent is needed
- FFR computation derived from coronary computed tomography angiography acquisition should include the entire heart, be performed according to a protocol to lower the heart rate without motion or misalignment
- FFR computation derived from invasive coronary angiogram require at least two different angiographic views without overlap, foreshortening, panning and with long, brisk contrast injections
- FFR computation derived from intracoronary imaging should cover all the lesions in the interrogated vessels
Fluoroscopic anatomy for the guidance of percutaneous transcatheter interventions
- Left-sided heart structures can be described by using 1,2,3 and 4 chamber views;
- Although fluoroscopic views can potentially differ between patients, average angulations can be established for description of left-sided heart structures;
- Standard or modified echocardiographic views mimicking fluoroscopic chamber views can be obtained by both transthoracic and transoesophageal echocardiography.
- The fluoroscopic right heart
- Right-sided heart structures can be described by using 1,2,3 and 4 chamber views;
- Two additional chamber views obtained in extreme LAO (lateral) views (i.e., bicaval and RVOT-PA chamber views) can be useful to visualize the atrial septum in plane and the right ventricular outflow tract;
- Standard or modified echocardiographic views mimicking fluoroscopic chamber views can be obtained by both transthoracic and transoesophageal echocardiography.
- The use 1,2,3 and 4 chamber views enable the operator in navigating the left side of the heart and targeting specific structures for transcatheter interventions;
- Intraprocedural use of MSCT-derived fluoroscopic angulations can particularly useful for the guidance of complex transcatheter procedures (e.g., edge-to-edge mitral valve repair, transcatheter mitral valve annuloplasty).
- Atrial septum and transseptal puncture
- The use 1,2,3 and 4 chamber views enable the operator in navigating the right side of the heart and targeting specific structures for transcatheter interventions;
- Intraprocedural use of MSCT-derived fluoroscopic angulations can particularly useful for navigating the right ventricle and and guiding transcatheter procedures targeting the tricuspid valve (e.g., edge-to-edge tricuspid valve repair, transcatheter tricuspid valve annuloplasty).
- Invasive coronary angiography is limited by the two-dimensional nature of fluoroscopy;
- Fluoroscopic coronary anatomy should be assessed in correlation with underlying cardiac wall and structure, using cardiac chambers view as reference patterns;
- As the frequency of use of diagnostic CTCA increases, it has the potential to provide additional information for planning and guiding coronary procedures based on 3D tomographic dataset.
Large animal models for the interventional cardiologist: a comparative anatomy, imaging, histopathology and regulatory perspective
Canines- Left atrial appendage ablation
- EP studies
- Pros:
- Heart anatomy is closer to human (valves, chordae, coronary system right heart dominant)
- Valve leaflets thicker
- Transoesophageal echocardiography is better
- Easily sourced at any weight
- Monogastric (per os…)
- Cons:
- Rapid growth
- More susceptible to infection, especially thorax
- High incidence of arrhythmia (anaesthesia)
- More difficult to handle
- Brawny animal (surgery)
- Hypertrophic ventricles
- Inflammation (more marked)
- Pros:
- Valve orifices & function similar to human
- More space around the mitral annulus
- Growth compatible with long-term studies
- Very robust & docile animal
- Prone to calcification in juvenile
- Cons:
- Heart anatomy less similar to human
- leaflets thin and fragile
- No aortic-mitral curtain
- Fibrillation is difficult to overcome
- More difficult to source at a given weight
- More expensive
- Ruminants (per os…)
The hybrid approach to CTO intervention
The steps of the hybrid approach to CTO crossing:- Dual injection
- Assessment of CTO characteristics
- Antegrade wiring
- Antegrade dissection/reentry
- The retrograde approach
- Change
- When to stop
- CTO modification when CTO crossing fails
The key components of angiographic review to guide CTO PCI:
- Proximal cap (clear or ambiguous location, tapered or blunt, side branches, calcification)
- Occlusion length and morphology (tortuosity, calcification, ambiguity of its course)
- Distal vessel (size, bifurcations, tortuosity, calcification)
- Potential retrograde options for reaching the distal true lumen, such as collaterals (type, size, tortuosity, entry and exit angle, distance between exit and distal cap) or aortocoronary bypass grafts
Spontaneous coronary artery dissections
Approach for diagnostically ambiguous casesIn cases of diagnostic uncertainty, the following approach can be useful:
- Reconsider the pre-test probability. For example, although SCAD can affect any age or sex, a higher index of suspicion is merited in male cases and patients at the extreme ends of the age spectrum (<30 or >80).
- Check for true lumen thrombus. SCAD does not appear to be highly thrombogenic and the presence of substantial true lumen thrombus should raise suspicion of an alternative diagnosis.
- Consider intracoronary (OCT) imaging.
- Assess for healing or evidence of atherosclerosis with follow-up CT Coronary Angiography (where spatial resolution allows).
- Consider other investigations (e.g. echo-bubble, prolonged ECG monitoring and thrombophilia screen – to assess probability of paradoxical embolism or intracardiac thrombus).
Revascularisation in SCAD
- PCI in SCAD is associated with an increased risk of complications, particularly iatrogenic dissection and haematoma propagation.
- Conservatively managed SCAD will usually heal with complete restoration of luminal architecture.
- A conservative approach is favoured where this is possible but PCI should be considered where there is significant myocardial jeopardy.
- Where PCI is required, care should be taken to minimise the risk of guiding catheter induced iatrogenic dissection and to ensure a correct luminal guidewire position.
- Despite the need for longer stent lengths and a higher risk of complications, improvements in coronary flow and good medium term outcomes can be achieved where PCI is required.
- CABG should be reserved for an emergency bail-out for extremely high risk scenarios.
Ischemia and myocardial infarction without obstructive coronary artery disease
- In the setting of INOCA two distinctive mechanisms play a central role (alone or in combination with CAD), defining different endotypes: CMD and epicardial vasospasm.
- In INOCA the main mechanisms of CMD are structural microcirculatory remodelling or vasomotor disorders caused by arteriolar dysregulation, the latter much related to endothelial dysfunction. The clinical manifestation of CMD in INOCA is MVA.
- Epicardial vasospasm originates from enhanced vessel reactivity to vasoconstrictor stimuli. The clinical manifestation of CMD is VSA.
- Non-invasive imaging techniques (TTE-DE, CMR, PET) are valid options to detect myocardial ischemia in patients without obstructive CAD.
- Interventional diagnostic procedures including guidewire testing and vasoreactivity testing should be implemented to differentiate between different INOCA endotypes: MVA, VSA, mixed angina and non-cardiac chest pain.
The COVID Pandemic and Interventional Practice
- STEMI patients should be brought to the CCL as rapidly as possible, and although door-to-balloon times are expected to be longer during the COVID-19 pandemic, a primary PCI strategy should remain the first choice.
- CCL must guarantee appropriate PPE for all personel and establish protocols with infection control to protect their staff and other patients
Robots in interventional cardiology
- Operators are subjected to cumulative effects of radiation exposure and orthopaedic injuries.
- The use of robotic technology not only makes PCI safer but may potentially revolutionize the way PCI is performed.
- In July 2012, the first R-PCI system, Corindus CorPath 200 obtained FDA clearance.
- CorPath GRX is the most advanced robotic PCI technology to date.
- Trials using mainly CorPath 200 system have proven R-PCI to be safe and feasible in simple to more challenging lesion subsets as compared to M-PCI.
CorPath GRX system
- Consists of:
- A mobile interventional workstation consisting of control console with touchscreen buttons and 3 joysticks (which controls the guide catheter, guidewires, and balloon/stent)
- Bedside unit composed of robotic drive with single use cassette, connected through a sleeve to guide catheter
- Can be used with both radial and femoral access
- Potential benefit for the patient:
- Increased procedural accuracy (accurate stent selection and less longitudinal geographic miss)
- Possibility of remote PCI in underserved areas
- Potential benefit for the operator:
- Improved ergonomics
- Reduced radiation exposure
Limitations of CorPath GRX system
- Vascular access, diagnostic coronary angiography and engagement of guide catheter have to be performed manually.
- Limited to rapid exchange devices only.
- Does not support planned coronary bifurcation stenting with two-stent approach.
Right and left heart catheterisation
Basic haemodynamics and pressure wave interpretation The basic understanding of pressure waveforms in the heart will provide the foundation for appreciating alterations during coronary interventions- Key points:
− From right heart haemodynamics, review and understand genesis of “a” and “v” waves in both the right atrial and left atrial pressure waveforms
− From left heart haemodynamics, appreciate the normal transvalvular pressure relationships and sequence of activation
− From the LV pressure waveform, identify diastolic left ventricular filling waveforms and those associated with pathologic conditions involving diastolic dysfunction and aortic valve regurgitation
Cardiac shunt calculations
• Cardiac shunt calculations require the determination of systemic flow, pulmonary flow and effective pulmonary blood flow
• With these three calculations, both left to right, right to left, and bidirectional shunting can be computed with facility
Diastolic dysfunction: haemodynamics
- Characteristic findings of pericardial disease and restrictive cardiomyopathy are the most prominent forms of diastolic dysfunction
- The impairment of ventricular filling is common to both entities manifested as a diastolic “dip and plateau” configuration
- The most specific differentiating features of the 2 disease states involve the dynamic respiratory interaction of left and right ventricular systolic pressure
- Concordant respiratory systolic pressure changes are associated with restrictive cardiomyopathy whereas discordant respiratory pressure changes are associated with constrictive pericardial disease
Vascular access
Femoral artery access- Puncture and sheath placement should be performed in the common femoral artery (CFA)
- The femoral bifurcation, external iliac and the inferior epigastric arteries must be avoided.
- The skin crease, maximum pulsation, and the inguinal ligament, can be misleading anatomical landmarks
- In cases of technical or anatomical difficulties, fluoroscopy or ultrasound guidance might be helpful to locate CFA
- Using fluoroscopy, the optimal landing zone for CFA is located between the centre line and the lower part of the femoral head
Femoral Artery Access Complications
- Puncture in the CFA is associated with less vascular complications than higher (external iliac artery) or lower (superficial femoral artery/profunda femoris) puncture
- Major femoral bleeding have decreased over the last decade with better access site management
- Bed rest for > 2 hours after femoral artery access is required and limits the risks of access-site bleeding and complications
- Vascular complications often requires transfusion, urgent surgical repair or percutaneous intervention and prolonged hospitalisation
Radial artery access
- The radial artery which is superficial with no adjacent nerve, allows easy compression with no need for bed rest
- Radial or ulnar artery access can be obtained by direct anterior wall puncture or through-and-through technique
- Anatomical variations of radial-brachial-subclavian axis may complicate or prevent catheter advancement or progression of the procedure.
- It is far easier to prevent radial artery spasm than treat it
Radial Artery Complications
- Access site bleeding is rare and easily managed
- Vascular complications are rare and do not require surgical repair
- Anticoagulation is required to reduce the rate of radial artery occlusion, even following diagnostic angiography
- Radial artery occlusion, although most of the time asymptomatic, can be associated with hand ischaemia, therefore its occurrence should be reduced by the use of heparin, smaller sheath sizes, and ‘patent-haemostasis’
- Compartment syndrome is a rare but limb-threatening complication of rapidly evolving forearm haematoma. This must be detected and managed aggressively to prevent the development of ischaemia
Current potential indications for left distal transradial access:
Right-handed patients
Left-handed patients with an:
Inaccessible proximal radial artery
Proximal radial vasospasm
Anatomically hostile right radial approach
The presence of an iatrogenic AV fistula in the right arm
Significant upper limb arthritis
Obesity
Requirement for LIMA graft angiography
Current contra-indications for left distal transradial access:
No palpable artery in the anatomical snuffbox
Distal radial artery minimum diameter <2mm
Emergency invasive coronary angiography/intervention during the learning curve
Left-sided hand venous cannula obstructing the snuffbox.
Tips and tricks for left distal transradial access
Ask the patient to flex the thumb under fully flexed fingers and apply mild ulnar flexion
Use the right femoral drape hole in the conventional fenestrated drape
Place support under the left arm to direct the pronated wrist as far toward the right groin as possible
Aim for an anterior wall puncture (to avoid injury to the bony floor of the snuffbox)
Use ultrasound to guide precise puncture.
Advance the guidewire under fluoroscopy (to avoid passage into the palmar arch)
All other aspects are identical to a conventional proximal radial approach to access
Access site and non-access site bleeding
- Major bleeding after femoral or transradial PCI is an independent predictor of mortality
- Radial access reduces substantially access-site related bleeding and complications
- The clinical impact of non-access site bleeding is stronger than access-site related bleeding
Vascular closure
Approach to femoral access and closure- Define the bony landmarks and palpate the common femoral artery
- Fluoroscopy to identify the medial half of the femoral head just inferior to the midline
- Confirm needle location prior to femoral artery entry using fluoroscopy
- Femoral angiography (RAO/LAO 30-40 degrees) to determine sheath entry site in relation to the femoral head, the inferior epigastric artery, and the CFA bifurcation
- Choose manual vs. VCD based on the size of the vessel, location of the arteriotomy, vessel calcification, PVD, and patient comorbidities, including risk of infection
Predictors of increased risk of vascular complications during PCI
- Increasing age
- Female sex
- Smaller individuals
- History of CABG, congestive heart failure, a bleeding disorder (haemophilia, thrombocytopeania, or disseminated intravascular coagulation), stroke, PVD, diabetes, chronic obstructive pulmonary disease, renal failure or a creatinine ≥2 mg/dL (>177 μmol/l), liver failure, immunosuppression
- Emergency procedure
- Multivessel coronary disease
- Complex coronary disease
- Multivessel PCI
- Use of an intra-aortic balloon pump
- GP 2b/3a antagonists
(Source: American Heart Association, Inc.)
Cardiac transseptal catheterisation
Conditions when transseptal puncture should not be undertaken- Thrombus at septum
- Atrial myxoma
- Tumour at septum
- Left atrial thrombus (usually)
- Bleeding diathesis
Routes to the right atrium
- right femoral vein
- left femoral vein
- right internal jugular vein
- transhepatic
Atrial septal anomalies that can cause difficulty
- resistant septum
- tender septum
- bulging septum
- giant LA
- very large RA
- atrial septal aneurysm
Alternatives to simple needle/catheter puncture
- Baylis RF catheter
- Electrosurgical cautery generator connected to needle
- Eximer laser
- SafeSept™ wire
- balloon dilatation
- Echocardiography (TOE or ICE) allows safe specific-site crossing for new left heart interventions
Complications of transseptal puncture
- atrial arrhythmias
- vasovagal reaction
- embolism
- puncture outside atrial cavities
- haemopericardium
- post-puncture atrial septal defect
Catheterisation for peripheral diagnostic and interventional procedures
Basic principles of peripheral angiography- Angiography can be performed in virtually all patients
- Procedural complications may increase in patients with advanced atherosclerosis
- Whenever possible, diseased vascular segments should not be used for vascular access
- In patients with end-stage renal disease upper extremity access should be avoided whenever possible
- Vascular access gained through prosthesis should be performed with caution
- Complications are related either to access or to contrast agents, or are the consequence of catheter manipulations
Basic principles to reduce the risk of non-access-related complications of diagnostic angiography:
- Perform high-flow injections through multiple-side-hole catheters
- Do not advance a catheter without a wire
- Make sure that the catheter tip is not in contact with the vessel wall before injecting
- Check sheaths and catheters for back-flow and flush them regularly
- For prolonged catheterisation consider periprocedural anticoagulation
- Caution while advancing hydrophilic wires
- Minimise catheter manipulations.
Key points for lower extremity angiography
- Pelvic angiography is necessary for the assessment of cross-over options
- Distal run-off angiography should always be performed prior to endovascular interventions in order to:
- have a complete diagnostic study;
- plan the intervention;
- estimate the probability of success;
- identify complications during revascularisation such as distal embolisation. - Multiple projections may be needed to make an adequate assessment of:
- the internal-external iliac bifurcation;
- the common femoral bifurcation;
- the distal popliteal trifurcation. - In patients with critical limb ischaemia, the angiographic study should include the foot circulation.
Angiography of the mesenteric and renal arteries
- Femoral approach is the most common
- If downward take-off of the vessels and intervention is planned, consider arm approach
- Left brachial approach is adequate for both diagnostic angiography and interventions
- Radial approach may be used for angiography - 125 cm catheters may be needed - but is not adequate in all patients for revascularisation
- Aortography prior to selective cannulation is recommended
Cardiac catheterisation in children and adults with grown-up congenital heart disease
Indications for catheterisation in children and adults with congenital heart disease- Insufficient or conflicting non-invasive data
- Unexpected and/or unexplained unfavourable clinical course
- Intended interventional treatment
Contraindications for catheterisation in children and adults with congenital heart disease
Absolute contraindications:
- Sufficient non-invasive information already available
- No previous non-invasive assessment
- Lack of potential therapeutic/management consequences as a result of catheterisation
- Uncontrolled coagulation disorder
- Sepsis or septic shock
- Severe hemodynamic compromise
Risks of catheterisation in children and adults with congenital heart disease
- Bleeding
- Thrombosis
- Trauma to vessels and cardiac structures
- Cardiac tamponade
- Arrhythmia
- Pulmonary or systemic embolism
- Allergic reactions
- Consequences of radiation exposure (children, young adults and females being especially prone to biological effects)
Principles of catheterisation in children and adults with congenital heart disease
- Meticulous indiviudual planning
- Selection of the least traumatic and most effective vascular access
- Maximal reduction of radiation exposure
- Combination with non-invasive imaging
- Combination of diagnostic and therapeutic procedures within one session
Considerations for diagnostic catheterisation in repaired coarctation
- Gradient across the site of repair
- Dimensions and anatomy (aneurysm, residual stenosis) at the level of repair
- Presence of collaterals
- Assessment of the aortic arch (especially the presence of hypoplasia or additional stenosis)
- Anatomy of head and neck vessels (including their origin in relation to residual lesions)
- Dilatation of the ascending aorta
- Presence of a bicuspid aortic valve, valvar stenosis or regurgitation
- Ventricular function
Considerations for diagnostic catheterisation in repaired tetralogy of Fallot
- Right ventricular size and function
- Degree of tricuspid regurgitation
- Dimensions of and gradient across the right ventricular outflow tract (obstruction/dilatation)
- Qualitative and and semiquantified assessment of pulmonary regurgitation
- Anatomy of branch pulmonary arteries
- Presence of a residual ventricular septal defect
- Presence of dilatation of the aortic root
Considerations for diagnostic catheterisation post arterial switch procedure
- Function of the neo-aortic and neo-pulmonary valves
- Transposed coronary arteries : assessment of possible coronary stenosis (ostial, proximal)
- Aortic root: assessment for possible dilatation
- Pulmonary and aortic anastomosis: assessment for possible supravalvular stenosis
- Pulmonary bifurcation and branch pulmonary arteries: anatomy and possible gradients
Considerations for diagnostic catheterisation post atrial switch procedure
- Assessment of right (systemic) ventricular function
- Assessment of tricuspid regurgitation
- Assessment for obstruction of the systemic and/or pulmonary venous return
- Presence of a left to right shunt or right to left shunt (including their location and size)
- Presence of a compromised coronary sinus
- Presence of left ventricular outflow tract obstruction
Endomyocardial biopsy
Aims in performing endomyocardial biopsy- Diagnose the underlying disease in patients with ongoing symptoms and non-ischaemic cardiomyopathy (including infiltrative cardiomyopathies) and/or myocarditis
- Enable appropriate individual decision making regarding specific and/or aggressive therapy regimens
- Obtain valuable data regarding future risk stratification
Suggested pre-intervention studies
- FBC, clotting studies (PT/INR, aPTT and anti-factor Xa, if required)
- A resting 12-lead ECG
- Transthoracic echocardiography and/or cardiovascular magnetic resonance imaging (CMR) study
Essential questions regarding the choice of bioptome
- Which ventricle should be biopsied (left vs. right ventricle)?
- Which access site is prefered (jugular vein vs. femoral vein vs. femoral artery vs. radial artery)?
- How many biopsy specimens are required?
Essentials in taking biopsy specimens
- Bioptome jaws have to be opened within the respective ventricular cavity “before” myocardial wall contact
- Close wall contact is achieved if a series of ventricular premature beats occurs
- After each biopsy sampling careful and repetitive flushing of the guiding sheath or guiding catheter is mandatory
Potential major complications of endomyocardial biopsy
- Pericardial tamponade with need for perciardiocentesis
- Haemo- and pneumopericardium
- Permanent AV-block requiring permanent pacemaker implantation
- Myocardial infarction
- Transient cerebral ischaemic attack and stroke
- Death
Suggested routine work-up of EMB samples
- Histopathological work-up comprising hematoxylin/eosin, Masson’s trichrome as well as Giemsa stains
- Immunohistochemistry using specific antibodies for detection of T-lymphocytes (e.g., CD3+) and macrophages (e.g., CD68+)
- Molecular pathological PCR analyses for detection of potential viral genomes
Limitations of endomyocardial biopsy
- Invasive procedure with an albeit low risk of complication
- Limited steerability of bioptomes preventing biopsy sampling in some areas
- Sampling error due to limited number of biopsy samples and limitation of sampling to subendocardial layers
Pericardiocentesis
Key echocardiographic findings in cardiac tamponade- Presence of a pericardial effusion
- Right atrial collapse in late diastole
- Right ventricular free wall collapse in early diastole
- Increase in E-wave velocity across tricuspid valve during inspiration
- Decrease in E-wave velocity across mitral valve during inspiration
- Inspiratory decrease and expiratory increase in diastolic pulmonary venous forward flow*
- Dilated inferior vena cava without inspiratory collapse
Key haemodynamic findings in cardiac tamponade
- Elevated right atrial pressure
- Elevated intra-pericardial pressure (very similar to right atrial pressure)
- Elevation and equalisation of left-right ventricular filling pressure
- Loss of y descent of the right atrial pressure waveform
- Arterial pulsus paradoxus (i.e., an inspiratory decrease in excess of 10 mmHg in systolic blood pressure)
Situations warranting special consideration before performing pericardiocentesis*
- Haemopericardium secondary to type A aortic dissection
- Traumatic haemopericardium
- Haemopericardium secondary to post-myocardial infarct ventricular free wall rupture
- Bleeding diathesis
--Use of anticoagulants
--Raised INR/APTT/PT
--Platelet count < 50,000 - Recurrent pericardial effusions
- Purulent pericardial effusions
- Small pericardial effusions that warrant drainage
- Loculated pericardial effusions
- Posteriorly located pericardial effusions difficult to access percutaneously
Techniques for confirming needle/catheter placement in the pericardial space*
- Monitor ECG signal from aspiration needle
−− ST segment elevation/PVCs suggest epicardial irritation or puncture
−− PR elevation/PACs suggest entry into RA - Monitor pressure
−− Intrapericardial pressure tracing observed (RV pressure waveform suggests entry into RV) - Inject agitated saline and observe for bubbles arriving in pericardial space with echocardiography
- Inject contrast under fluoroscopic screening
- Advance an 0.035-inch J wire and observe it wrapping around heart using fluoroscopy
Post-pericardiocentesis management*
- Close monitoring and observation
- Remain vigilant for development of complications of pericardiocentesis
- Post-procedure CXR to exclude pneumothorax
- Analgesia as required for pericardial pain
- Catheter drainage: free drainage or intermittent aspiration
- Record volume draining at regular intervals
- Strict aseptic technique for catheter manipulations
- Flush with heparinised saline every 6-8 hours
- Minimise duration of catheter stay to reduce risk of infection
- Pull catheter as soon as appropriate or when volume draining is <25-50mls/24 hours
- Pull catheter in event of fever/sepsis
- TTE before pulling catheter
- Surveillance TTE at appropriate intervals following catheter removal
- Immediate TTE in event of deterioration in patient’s haemodynamics
Management strategies for recurrent symptomatic pericardial effusions*
- Repeat closed pericardiocentesis
- Percutaneous balloon pericardiotomy
- Surgical pericardial window creation
- Intrapericardial injection of sclerosing agents
- Adjuvant local and/or systemic chemotherapy for malignant effusions
- Adjuvant radiation therapy (external or with intrapericardial radionuclides)
- Combination of above strategies
Novel percutaneous pericardial interventions
- Percutaneous balloon pericardiotomy
- Percutaneous pericardial biopsy
- Pericardioscopy
- Percutaneous pericardial access for epicardial mapping and ablation of ventricular and supraventricular arrhythmias
- Left atrial appendage occlusion
- Intrapericardial infusions for recurrent pericarditis
Percutaneous ventricular assistance
Therapeutic aims of PVAD- Augmentation of cardiac output
- Augmentation of mean arterial pressure
- Increase in myocardial ischaemic threshold
- Ventricular unloading
IABP insertion
- percutaneous femoral arterial access
- passive cardiac support and increase in ischaemic threshold
- balloon sizing according to height:
- <160 cm:34 ml balloon,
- 160-182 cm:40 ml balloon,
- <182 cm:50 ml balloon
- balloon tip should be placed distal to the left subclavian artery at the level of the carina
TandemHeart™
- Venous, arterial and transseptal access are required
- Provides active cardiac support with increased flow up to 5 L/min achievable
- Systemic heparinisation necessary to prevent thromboembolic complications
- Function not dependent on stable cardiac rhythm
- Insertion requires experience and multidisciplinary co-operation
Impella®
- Can be used for left or right ventricular assistance
- Active cardiac support provided with flow rates of 2.5-5 L/min
- Functions independent of a stable cardiac rhythm
- Impella LP 2.5 and CP can be inserted percutaneously without a surgical approach
Radiation protection
Radiation in context- X-rays are a proven carcinogen
- Effective dose from medical radiation is 150 chest x-rays per head per year
- In cardiology patients, about 50% of the cumulative dose is from invasive cardiology
- Interventional cardiologists receive annual exposure 3-times higher than radiologists
- Unnecessary medical radiation exposure is an avoidable health burden
Average dose comparisons for common examinations (by equivalent chest x-rays)
- 250: diagnostic coronary angiography
- 500: abdominal arteriography
- 500-2500: coronary stenting or cardiac radiofrequency ablation
- >2500: dilation of chronic total occlusion of coronary artery
Exposure doses for high volume interventional cardiologist
- Average: 250 chest x-rays per operator per year (below apron)
- Left side > right side
- Reduced by 90% with proper protection policy
The risks of radiation
- Deterministic (skin effects, from epilation in doctors to dermal necrosis in patients)
- Stochastic (cancer in doctors and patients)
- Stochastic, but traditionally considered deterministic (eye cataract in 50% of doctors)
Pregnant cardiologists and pregnant patients
- In utero exposure to ionising radiation can be teratogenic and carcinogenic
- Teratogenic effects are deterministic and require a threshold >50 mSv
- The stochastic risk of cancer (mainly leukaemia) is increased with increasing doses, but no safe limit exists
- Occupational dose limit is <5 mSv for the entire pregnancy for NCRP (in USA)
- A more restrictive limit of <1 mSv for the entire pregnancy is set by ICRP and IAEA (in Europe)
- A 5 mSv dose to the foetus increases the lifetime cancer risk of 1 in 500 (above the normal lifetime cancer risk of 40% to 50%)
- More data are needed to assess (cancer and non-cancer, acute and long term) effects of radiation exposure of mothers (and fathers!) on offspring
- The best protection and surveillance for pregnant operator is achieved with double thickness of protection garment; specific maternity lead apron; and monthly monitoring of the radiation exposure under the lead at waist level
How to maximise protection
- Time (cine mode gives 10-times more radiation exposure than fluoroscopy)
- Distance (inverse square law)
- Shielding (structural, mobile, personal and cultural)
Radiation protection in the cardiac catheter laboratory:
the 3 A’s strategy
- Awareness of risks
- Appropriateness of examinations
- Audit of dose to patient and operators
How to maximise protection
- Ask the patient or family about previous radiation (link to imaging record). Answer questions about radiation safety (link to patient brochure)
- Use ultrasound when possible
- Position hanging table shields and overhead lead shields prior to procedure with reminders during the case as needed
- Operators and personnel wear well fitted lead aprons, thyroid shield and leaded eye wear
- Use pulse rather than continuous fluoroscopy when possible, and with as low a pulse as possible
- Position and collimate with fluoroscopy off, tapping on the pedal to check position
- Collimate tightly. Exclude eyes, thyroid, breast, gonads when possible
- Operator and personnel hands out of the beam
- Step lightly: tap on pedal and review anatomy on last image hold rather than with live fluoroscopy when possible; minimise live fluoroscopy time
- Minimise use of electronic magnification; use digital zoom whenever possible
- Acknowledge fluoroscopy timing alerts during procedure
- Use last image hold whenever possible instead of exposures
- Adjust acquisition parameters to achieve lowest dose necessary to accomplish procedure: use lowest dose protocol possible for patient size, lower frame rate, minimise magnification, reduce length of run
- Plan and communicate number and timing of acquisitions, contrast parameters, patient positioning and suspension of respiration with radiology and sedation team in advance to minimise improper or unneeded runs
- Move table away from x-ray tube in both planes. Move patients as close to detector in both planes
- Use power injector or extension tubing if hand injecting
- Move personnel away from table or behind protective shields during acquisitions
- Minimise overlap of fields on subsequent acquisitions
- After procedure: record and review dose
Sedation, pain management and resuscitation
Background- A growing number of procedures are performed outside the operating room
- Sedation and/or analgesia make the procedures possible and acceptable to patients
- Sedation and/or analgesia should be provided by trained and skilled personnel.
Definitions
- Sedation and anaesthesia comprise a continuum of states ranging from minimal sedation (anxiolysis) to general anaesthesia
- Achieving the intended level of sedation and analgesia is not always straightforward
- Practitioners should always be able to rescue patients achieving a level of sedation deeper than intended
GOALS OF SEDATION AND ANALGESIA
- Maintain patient safety and welfare
- Minimize physical pain and maximize patient comfort
- Control anxiety and, minimize psychological trauma
- Control behavioral movement to allow safe performance of procedures
Patient monitoring
- Every patient undergoing sedation and/or analgesia should be monitored by a trained person, whose primary and only task is monitoring of the patient
- Standard monitoring must be applied to all patients undergoing sedation and/or analgesia
- All standard monitoring equipment and medication as well as all emergency equipment (the light on the laryngoscope!) and medication should be checked daily (by trained staff) and after each resuscitation event
Practice of sedation and analgesia
- Sedation and/or analgesia are preferably given intravenously in small incremental doses
- Sufficient time must elapse before incremental doses are given
- Hypnotics and analgesia medication for which reversal agents are available are first choice
- Reversal agents should always be readily available
- Recovery time should be adequate, using formal discharge criteria, especially when sedation has been reversed
Anti-emetics
- Prophylaxis of postoperative nausea and vomiting with dexamethasone and 5-HT3-antagonists
- Treatment of postoperative nausea and vomiting with metoclopramide and 5-HT3-antagonists
Recovery
- After the procedure, the patient must be monitored in a recovery area for a sufficient time
- The recovery area must be adequately equipped
Resuscitation
- Resuscitation should follow recent guidelines [38, 47]
- Required equipment should be at hand as recommended by the ASA
- Mechanical chest compression devices may offer special benefits in the cardiac catheterisation laboratory
Biostatistics for the interventionist
Significance testing, estimation and confidence intervals- Significance testing, estimating treatment effects and confidence intervals are at the heart of statistical inference
- The p-values from significance tests do not prove that a treatment works (or doesn’t work), but rather provide a measure of the strength of evidence against the null hypothesis being true
- Estimates of relative and absolute treatment benefit as well as the underlying risk should be considered
- Confidence intervals should always be calculated to provide a range of plausible values for the true treatment effect
Time-to-event outcomes
- Many trials study time to the first occurrence of an event of interest
- In such trials, patients are not all followed for the same period of time
- The most common model used for time-to-event data is the Cox proportional hazards model, with the hazard ratio as the measure of treatment effect
- Kaplan-Meier plots display the cumulative proportion of patients surviving or failing over the follow-up period
Quantitative outcomes
- Clinical trials analysing quantitative outcomes typically use the two-sample t-test to test for a difference in means
- The key information required for the two-sample t-test is the mean value, standard deviation and number of observations in each group
- Where baseline values of the outcome have been measured analysis of covariance or linear regression should be used
- When the outcome is very skewed, non-parametric methods should be used
Non-inferiority trials
- The goal of NI trials is to demonstrate that a new treatment is no worse than the existing treatment by a pre-specified difference
- The focus in NI trials tends to be on confidence intervals rather than hypothesis testing
- The choice of the margin of non-inferiority should involve a combination of statistical reasoning and clinical judgement
- The control group should be the best available established treatment for the condition being studied
Sample size and power
- Determining the number of patients required to demonstrate a treatment difference is called the sample size calculation
- The power of a study is the probability of rejecting the null hypothesis if the treatment really works
- A Type-2 error is the probability of not detecting a real treatment difference
- All else being equal, larger trials provide more power and precision
- A smaller treatment effect will require a larger sample size, all else being equal
Baseline covariate adjustment
- Baseline covariates are variables collected before randomisation and which are associated with the primary outcome
- Adjustment for prognostic baseline variables can lead to gains in terms of less biased and more precise estimates of the treatment effect
- The choice of which covariates to adjust for should be clearly pre-specified in the SAP and should not be based on statistical tests for baseline imbalance
Secondary endpoints and subgroup analyses
- The probability of finding a statistically significant result by chance increases with the number of significance tests carried out
- Most emphasis should be placed on the results of the primary endpoint
- Results from secondary or tertiary endpoints and subgroup analyses should be interpreted with caution
- Subgroup analyses should be pre-specified and always present results of an interaction test – though bear in mind that such tests lack power
- Significant subgroup interactions should be considered in the light of external evidence, biological plausibility and number of subgroups investigated
Composite endpoints
- CEPs are commonly used in cardiovascular clinical trials to increase power
- Results of trials involving CEPs need to be interpreted with caution
- In addition to the primary results for the CEP investigators should report results for the individual components of the composite
- Is the overall positive result being driven by the least clinically important component of the CEP?
- The win ratio takes into account clinical importance of the component events and enables different types of endpoints to be combined
Cardiac biomarkers
What does a raised troponin mean?- Elevations of cardiac troponin indicate the presence of irreversible myocardial damage and are not specific for acute myocardial infarction where the mechanism is myocardial ischaemia
- A troponin result should not therefore be interpreted without the clinical context and the kinetic change during serial sampling
High-sensitivity troponin assays
- More sensitive troponin assays will detect more patients with acute or chronic myocardial damage, and at earlier stages of disease
- These small elevations of troponin are associated with an adverse prognosis, regardless of whether troponin is due to ACS or due to one of the numerous differential diagnoses
- Therefore, the underlying reason should be actively searched for as soon as possible to warrant early start of a specific therapy
Early rule-out for Myocardial infarction
-
The advent of more sensitive cTn assays which allow use of cTn at lower decision cut-offs with appropriate imprecision (10%CV at the 99th percentile cut-off) obviate the need for additional biomarker that detect myocardial necrosis earlier
- A faster diagnostic protocol with re-testing of cTn at 0/3 hours is altready recommended as the standard of care when a hsTn assay is available.
- Faster diagnostic protocols with re-testing of cTn are recommended as an alternative if validated hsTn assays are being used.
As an additional option, copeptin combined with a conventional cTn may rule-out of MI based on a single blood draw at presentation. This strategy could also help to guide safe discharge of patients after rule-out.
Troponin and infarct size
- The cumulative release of cardiac constituents reflects the total amount of myocardial necrosis
- More conveniently, infarct size may be estimated by single time-point measurement of cTn
- There is good correlation between infarct size and cTn at any time beyond the first 24 hours after onset of symptoms
- Correlation between cTn and infarct size is better for STEMI or larger infarct than for non-STEMI or more small infarcts
- 2014 ACC/AHA guidelines state that it may be reasonable to remeasure troponin once on day 3 or day 4 in patients with MI as an index of infarct size
Biomarkers and ACS risk stratification
Numerous biomarkers have been found useful for risk stratification of ACS
- Most evidence is available for cardiac troponins, inflammation proteins such as C-reactive protein, fibrinogen, natriuretic peptides, and markers of renal dysfunction
- Whilst elevation of cardiac troponin indicates the risk for acute (thrombotic) events such as death, MI during the first 30 days, inflammatory markers, natriuretic peptides and impaired renal function are associated with long-term outcomes
- So far, few biomarkers including cardiac troponins and natriuretic peptides are being recommended by practice guidelines
Troponin and therapy for ACS
- Whether a patient will benefit from more effective antithrombotic or antiplatelet therapy, or will derive benefits from early invasive vs. selected invasive therapy strongly depends on risk assessment
- Benefits of therapy are almost exclusively restricted to patients with high risk, or intermediate-to-high risk profile.
- Traditionally, cardiac troponins have been used for guidance of therapy and selection of invasive strategy
- Global risk can also be estimated by clinical multivariable scores such as the GRACE score
Periprocedural MI
- Diagnosis of a type 4 MI after elective PCI should be confirmed if the troponin was normal before PCI and rises to >5 times 99th percentile value within 24 hours post PCI and only in the presence of additional signs or symptoms of myocardial ischemia such as symptoms, ECG changes, new wall motion abnormalities on echo, or loss of viable myocardium. Otherwise, any postprocedural cTn elevation should be labelled as myocardial injury and not as type IV MI.
- In ACS type 4 MI is difficult to assess unless cTn before PCI is negative in two consecutive samples taken at least 6 hours apart
- Reinfarction in the first hours after PCI (as long as cTn is rising) is difficult to assess
- In cases with falling cTn values, an increase of 20% or more suggests re-infarction
- For the diagnosis, the clinical picture and ECG changes should ideally be considered
Fundamentals of coronary biomechanics
Terminology- Shear stress is the frictional force per unit area that the blood flow exerts on the vessel wall. Shear stress depends of the viscosity of blood and the blood flow velocity distribution – more specifically the shear rate – near the wall. Viscosity is a measure for the “thickness” of the fluid, while the shear rate is used to quantify the rate at which adjacent fluid layers move with respect to each other
- Vessel wall stress is the force per unit area within the tissue, caused by for example blood pressure. The deformation of the tissue is called strain when quantified per unit of length
Shear stress and early atherosclerosis
- The coronary arterial tree has many curved vessel segments and contains numerous bifurcations, leading to complex flow patterns with swirling flow, flow separation and flow reversal
- Heterogeneous shear stress distribution creates regions of low and high stress
- The low shear stress regions are prone to develop atherosclerosis, while normal and high shear stress levels create an atheroprotective environment
Shear stress and vulnerable plaques
- Atherosclerotic plaques modify the shear stress
- Elevated shear stress levels exist upstream and at the throat of the plaque, while downstream low shear stress prevails
- Rupture of vulnerable plaques mainly occurs in the upstream and throat region
- Shear stress has no direct mechanical effect on plaque rupture, but high shear stress may affect vulnerable plaque composition so as to enhance plaque vulnerability
How can we determine shear stress?
- Shear stress in human coronary arteries cannot be measured direclty, due to the size and movement of the coronary arteries
- Computational fluid dynamics can be applied to obtain the local velocity and shear stress distribution based on 3D imaging techniques
- The most accurate 3D reconstruction techniques rely on a combination of intravascular ultrasound and biplane angiography or multislice computer tomography ( Figure 6 and Figure 7)
- Combining imaging and computations allows us to study the relationship between shear stress, plaque localisation and progression and in-stent restenosis
Elastic behavior of vascular tissue
- Arterial tissue displays a nonlinear elastic behaviour as reflected by the J-shaped stress-strain curve shown in Figure 9
- Arterial tissue becomes stiffer as deformations get larger
- This behavior is due to embedded collagen fibers that get more and more aligned as the deformation enlarges, leading to a gradually increasing resistance of the tissue
Measurement of vessel wall strain
- In vivo measurement of strain in coronary arteries is feasible using intravascular ultrasound. Such measurements have been used to assess relative differences in strain to identify zones of large (normal tissue, soft plaque) and small deformation (hard plaque) can be measured
- A numerical technique, called Finite Element Analysis, can also be used to study stress and strain. This approach requires input regarding the mechanical behavior of the tissue and can be used to quantify the occurring strains and stresses during, for example, final kissing balloon inflation (see Figure 12 )
Current and future applications of virtual vessel wall stress analysis
- Wall stress analysis using finite element simulations is mainly limited to basic research
- Stress patterns in different types of plaques have been reported and the impact of stent design on the resulting wall stresses has been evaluated
- The feasibility of virtually implanting stents in patient-based coronary artery models has been demonstrated
- A patient-specific modeling approach will allow to gain insights into the actual real-life mechanics of the stents and their surrounding tissues and might for example help to formulate guidelines on how to further reduce the risk
- of stent fracture
Non-invasive imaging for coronary disease
Non-invasive imaging and coronary disease- Imaging is useful to confirm the diagnosis of coronary artery disease in patients with intermediate pre-test likelihood of disease
- While non-invasive angiography can reliably rule out the presence of obstructive coronary artery disease, demonstration of myocardial ischaemia with the use of functional testing is recommended before elective invasive procedures
- Combined and hybrid imaging with anatomical and functional imaging modalities is attractive for comprehensive evaluation of anatomy and functional significance of coronary stenosis
Coronary computed tomography angiography
- Coronary computed tomography angiography has become a routine clinical tool for the non-invasive evaluation of the lumen and walls of the coronary arteries with acceptable radiation dose
- Computed tomography angiography can reliably rule out the presence of obstructive coronary artery disease in the presence of low to intermediate pre-test likelihood
- Artefacts caused by coronary calcification or irregular heart rate constitute problems for computed tomography angiography
Myocardial ischaemia
- Documentation of ischaemia using functional testing is strongly recommended before elective invasive procedures for coronary artery disease
- Stress echocardiography and SPECT perfusion imaging are the most well-established techniques for the detection of myocardial ischaemia, but a growing amount of data about cardiovascular MR and PET is becoming available
- Detection of a large area of myocardial ischaemia by functional imaging is associated with impaired prognosis of patients
Myocardial viability
- The presence of dysfunctional but viable myocardium identifies patients who are most likely to benefit from coronary revascularisation
- Nuclear imaging, stress echo and contrast-enhanced MR techniques can be used to differentiate between viable myocardium and scar
Non-invasive imaging for structural heart disease
Key points before, during and after TAVI
Before TAVI:
- Confirmation of aortic stenosis severity
- Clinical evaluation and assessment of the risk of surgery
- Aortic valve annular dimensions for evaluation of prosthesis size selection
- Peripheral artery anatomy evaluation for planning procedural approach
- Evaluation of contraindications: aneurysm of ascending aorta (self-expandable prosthesis), intracavitary thrombus, coronary artery disease not amenable for percutaneous coronary intervention
- Echocardiography is the non-invasive imaging technique most frequently used to evaluate candidates for TAVI
- MDCT provides the most comprehensive pre procedural planning before TAVI including patient eligibility, device selection, device sizing and vascular access suitability.
During TAVI:
- Fluoroscopy, invasive hemodynamic, quantitative aortography and transoesophageal echocardiography are complementary tools used for procedural guidance
- The minimalist TAVI approach using fluoroscopy without TOE/general anaesthesia is widely used as the standard approach in many experienced high volume centers.
- Aortic valve crossing, balloon dilatation and positioning and deployment of the prosthesis are the key procedural steps
- Videodensitometric quantitative aortography provides accurate estimation of PVL grade and can guide the need for corrective manoeuvres for treating significant post-TAVI PVL including balloon post dilatation.
After TAVI:
- Confirmation of position and function of the prosthesis
- Echocardiography is the preferred method to evaluate presence and severity of paravalvular leakage
- MRI 2D flow phase contrast or 4D flow could be used for accurate quantification of residual post TAVI aortic regurgitation.
- MDCT is used for detection of reduced leaflet motion and subclinical leaflet thrombosis.
- Evaluation of complications: pericardial effusion, detection of new left ventricular wall motion abnormalities that may indicate occlusion of coronary ostia, stroke, vascular complications
Imaging for peripheral artery disease
Digital subtraction angiography- DSA is the gold standard for imaging PAD
- In intermittent claudication: image arteries from distal aorta until the ankles in both legs
- In critical limb ischaemia: image the affected side only and add a lateral DSA of the foot (pedal) arteries
- Selective injections and invasive pressure measurements may resolve remaining diagnostic questions on the significance of a stenosis
- Complications at puncture site occur in 0.04-1.5% of cases
- Catheter-induced complications occur in 0.4-1.0% of cases
- Adverse effects of iodinated contrast media include : anaphylactic reactions and nephrotoxicity (especially in patients with chronic kidney disease)
MR angiography
- First-pass contrast-enhanced MR angiography is accurate for imaging PAD and is available in all modern radiology departments
- Time-resolved MR sequences are helpful in imaging the lower leg and foot arteries in critical limb ischaemia
- Claustrophobia and pacemakers are contraindications for MR angiography
- Vascular metallic stents preclude standard MR angiography because of signal voids
- MR imaging problems are related to venous contamination, motion artefacts and less than optimal robustness of the method
- Nephrogenic systemic fibrosis (NSF) is a rare but potentially dangerous complication of gadolinium-based MR-contrast agents. NSF has only appeared in patients with very poor kidney function, i.e., a glomerular filtration rate of 30 ml/min/1.73 m2 or less
CT angiography
- Contrast-enhanced CT angiography is robust and accurate for the imaging of PAD
- Good spatial resolution makes for sharp, crisp images of the peripheral arteries
- Decreased accuracy of CT angiography in calcified vessels
- Imaging of in-stent vessel lumen is possible, though stainless steel stents may pose a problem
- Problems of iodinated contrast media: anaphylactic reaction and nephrotoxicity especially in patients with chronic kidney disease
Duplex Doppler ultrasound
- Duplex Doppler ultrasound (DUS) identifies haemodynamically significant artery stenosis by quantifying abnormally high blood flow velocities
- Doppler waveform analysis provides additional proof of significant artery stenosis
- Avoids both nephrotoxic contrast agents and ionising radiation
- Bowel gas and obesity may hamper evaluation of iliac arteries
- Not reliable in below-the-knee arteries
- Accuracy depends on the operator and cannot be checked afterwards
- Major value during pre-treatment work-up as additional means to decide whether an ambiguous obstruction at imaging is a significant stenosis and as a follow-up examination after endovascular or surgical treatment
Relative strengths and weaknesses of DSA, CT and MR angiography and DUS
- Digital subtraction angiography (DSA) is the reference standard for imaging PAD. DSA may not, however, identify patent vessel segments distal to long occlusions that can be seen with MR and CT angiography. DSA is an invasive study and more costly. Contrast load is an issue especially in patients with chronic kidney disease
- CT angiography is the most cost-effective imaging modality in PAD patients with adequate renal function and without extensive vessel calcifications. CT angiography allows evaluation of in-stent restenosis. Contrast load is an issue especially in patients with chronic kidney disease
- The advantages of MR angiography are in imaging PAD in extensively calcified vessels and, with the addition of time-resolved MR sequences, in dynamic evaluation of the lower leg and pedal arteries. A drawback is MR angiography’s suboptimal robustness. MR angiography does not allow evaluation of in-stent restenosis. MR angiography is contraindicated in patients with a pacemaker and in claustrophobic patients
- Duplex Doppler ultrasound (DUS) is a rapid and readily available technique to assess haemodynamically significant arterial stenosis. However, DUS has major shortcomings and the use of DUS as the initial imaging test in PAD has proved to be more expensive and less cost-effective thanthat of an MR- or CT-angiography first strategy
Invasive haemodynamic assessment
Haemodynamics of aortic stenosis- Invasive haemodynamic evaluation of aortic stenosis is only indicated in symptomatic patients when there is a discrepancy between the clinical and echocardiographic or non-invasive findings, or when such findings is nondiagnostic.
- Aortic stenosis should be assessed in the catheterisation laboratory with simultaneous measurement of central aortic and left ventricular pressures for the mean gradient, and with calculation of cardiac output.
- Aortic regurgitation will lead to an underestimation of the valve area.
- Dobutamine challenge should be performed in symptomatic patients with low-output, low-gradient aortic stenosis to determine the true severity of the valve lesion.
- Hemodynamic cardiac catheterisation can be helpful to confirm the diagnosis of paradoxical LF-LG AS, especially when there is discrepancy between non-invasive tests and clinical findings.
Angiography in valve regurgitation
- Angiography for valvular regurgitation is indicated in symptomatic patients when there is a discrepancy between the clinical findings and severity of regurgitation on echocardiography.
- Sellers’ criteria are the semi-quantitative method for assessing the severity of valvular regurgitation.
Haemodynamics in hypertrophic cardiomyopathy
- Invasive haemodynamic evaluation is indicated in symptomatic HCM patients when there is uncertainty regarding the presence or severity of the LVOT gradient.
- The best method for assessing the LVOT gradient in HCM is transseptal puncture to avoid ventricular entrapment.
- On the post-ectopic beat in HCM, the hallmark haemodynamic findings of dynamic LVOT obstruction are a decrease in the aortic pulse pressure with exaggeration of the “spike-and-dome” configuration.
- Provocative manoeuvres, such as Valsalva strain and isoproterenol administration, should be performed to detect the presence of latent LVOT obstruction.
Invasive physiological assessment of coronary disease (FFR)
Special features of FFR- Unequivocal normal value of 1.0
- Well-defined cut-off value (0.75-0.80)
- Independent of heart rate, blood pressure, and myocardial contractility
- Takes into account collateral flow
- Takes into account amount of viable myocardial mass
- No need for a normal coronary artery to compare with
- Higher spatial resolution than any other functional test
- High reproducibility
- Easily obtainable
- Linearly related to maximum blood flow
- Suitable to assess improvement by PCI
Lesion subsets in which FFR is applicable
- Intermediate coronary artery stenosis (angiographic severity 50-90%)
- Single-vessel disease
- Multivessel disease
- Left main stenosis
- Ostial and side branch stenosis
- Non-culprit stenosis in acute coronary syndromes
- Sequential stenoses
- Diffuse coronary disease
Pitfalls and limitations of NHPR (including iwFR, dPR, RFR)
- Resting indicies including iwFR, dPR and RFR have only been compared with FFR and independent studies to show improved outcome have never been performed.
- In proximal stenoses in large coronary arteries, false-negative NHPR is present in up to 30% of patients.
- False-negative NHPR are likely be present in case of a large perfusion territory, short tight lesion, young patients with good microvascular function, LM disease, or dominant right coronary arteries.
- Hyperemic gradients are 2 to 3 times larger than resting gradients. Therefore, avoiding hyperemia decreases the signal-to-noise ratio of the pressure pull-back recording and the sensitivity to unmask the significance of diffuse disease and cross-talk between different lesions in 1 coronary artery.
- The decreased signal-to-noise ratio at rest also enhances confounding by drift. Since drift is an absolute phenomenon (mm Hg/unit of time), its influence is larger when using resting indicies.
- Physiological assessment by resting indicies is not possible after PCI. A variable state of submaximal hyperaemia often exists for a prolonged time after PCI. Therefore, resting indicies do also not allow quantification of the rate of improvement by stenting.
Assessment of coronary vasoreactivity and the microcirculation
Endothelium-derived vasoactive substances- Endothelium-derived vasoactive substances play a key role in regulating vascular tone and function in response to a variety of agonists as well as shear stress
- Nitric oxide is the main vasodilating and endothelin the main vasoconstricting substance
Any imbalance between vasodilatating and vasoconstricting factors lead to endothelial dysfunction, a condition with systemic implications and associated with morbidity and mortality. In atherosclerotic coronary arteries endothelin is the most important contributor to endothelial dysfunction and promotes vasoconstriction, cellular proliferation and angiogenesis.
The coronary microcirculation is essential for adapting vascular resistance and thus guiding blood flow to the different parts of the heart, according to its needs. In fact, contrary to the epicardial vessels, microcirculatory vessels are the main contributors to vascular resistance, especially the pre-arterioles. The maximal increase in coronary blood flow to stimuli such as exercise, mental stress or pharmacologic agonists is referred to as coronary flow reserve.
Epicardial vascular function can be assessed by intracoronary infusion of vasoactive substances such as acetylcholine or nitroglycerin as well as by physiological interventions such as exercise or the cold pressor test. Changes in coronary artery diameter or area are assessed by quantitative coronary angiography.
Microcirculation cannot be displayed directly, but functional assessment is possible by the assumption that it is the main determinant of the regulation of coronary blood flow. Techniques in the catheterizations laboratory (angiographic frame counts, intracoronary or coronary sinus thermodilution, and intracoronary Doppler measurements), as well as other functional tests (Transthoracic echocardiography Doppler, Positron Emission Tomography or CMR) are used clinically to quantify blood flow changes.
Less invasive techniques to assess endothelial dysfunction have been developed. The most important are the measurement of brachial artery flow-mediated vasodilation by ultrasound, the measurement of changes in the forearm blood flow by plethysmography, as well as the assessment of pulsatile arterial volume changes with finger plethysmography (EndoPAT) and the dynamic assessment of the retinal vessels (DVA).
Epicardial endothelial dysfunction is seen in almost every condition associated with atherosclerosis and gives important prognostic information. Although atherosclerosis is a diffuse and systemic disease, epicardial vascular dysfunction is often segmental and those segments are especially vulnerable of plaque development, rupture and thrombus formation.
Intracardiac echocardiography
Comparison of the two types of intracardiac ultrasound systems
Optical coherence tomography
Introduction- Optical coherence tomography (OCT) is a light-based imaging modality offering a 10 times higher image resolution (axial resolution 15 μm) compared to intravascular ultrasound (IVUS) by using near infrared light with a centre wavelength of 1,300 nm rather than sound in the megahertz range
-
This high resolution, however, is at the expense of a reduced penetration depth into tissue and the need transiently to create a blood-free field of view during image acquisition
-
Protoypic “time domain OCT” has been replaced by “Fourier domain OCT” devices
- Image acquisition only requires a couple of seconds (typically 3 sec for a pullback through an artery segment of 60 mm length), thus alleviating imaging-related ischaemia seen with time-domain OCT
Physical principles
- The basic imaging principle is analogous to pulse-echo ultrasound
- imaging OCT uses infrared light waves to reflect off the internal microstructure within the biological tissues
- The echo time delay of the emitted light is used to generate spatial image information, and the intensity of the received (reflected or scattered) light is translated into a (false) color map
- As the speed of light is much faster than that of sound, an interferometer is required to measure the backscattered light
- The interferogram is detected as a function of wavelength, either by using a broadband source as in the time domain systems, and spectrally resolved detection, or alternatively by incorporating a novel wavelength-swept laser source called “swept source OCT”, or optical frequency domain imaging (OFDI)
- Current Fourier domain OCT systems produce images much faster than standard video-rate. and can scan 200-500 angles per revolution (frame), and 5-10 images per mm in a pullback, with 20 mm/sec (or higher) pullback speeds
Practical application in the catheter laboratory
- After administration of intracoronary nitrates, the OCT imaging catheter is advanced distally into the coronary artery over the angioplasty guidewire (0.014”)
- Care should be taken to position the guide catheter coaxially
- Automated OCT pullback (20 mm/sec) is performed during flush administration
- The preferred flush is iso-osmolar contrast medium at 37 °C using a power injector (flow rate 3 ml/sec) connected to the standard Y-piece of the guiding catheter
OCT assessment of atherosclerotic lesions
- OCT has the ability to characterise the structure and extent of coronary artery disease in unprecedented detail
- OCT is capable of reliably differentiating normal vessel wall from various components of atherosclerotic plaques, including fibrous, calcified or lipid-rich tissues
- OCT can visualise features associated with risk of plaque rupture, including thin-cap fibro-atheroma, plaques with large lipid components, macrophage infiltration and calcified nodules with disruption
- OCT can identify the mechanism of ACS. At culprit sites fresh thrombus is commonly observed
Use of OCT to guide coronary interventions
- The baseline use of OCT alter the interventional strategy, leading to selection of different stent lengths and diameters
- The use of OCT post-intervention can reveal suboptimal stent deployment
- The application of OCT metrics of suboptimal stenting identifies patients at higher risk of major cardiovascular events during follow-up
Near-infrared spectroscopy
Invasive direct coronary imaging- Coronary angiography gives a semi-quantitative assessment of percent diameter stenosis
- Coronary angiography provides no quantitative or qualitative information on atheroma burden or plaque composition
- LCP has important implications for plaque progression, stability and may influence the outcome of PCI
- Present and future direct multi-modality direct coronary imaging gives accurate information on atheroma architecture as well as composition and is likely to become a standard tool for invasive evaluation and therapy
Principles of operation and validation
- The NIRS catheter is easy to use and has been rigorously validated against histopathology for the detection of LCP
- Ultrafast laser scanning mitigates against cardiac motion artefact
- Positively identifies lipid composition whereas ultrasound relies on acoustic shadowing
Potential clinical uses for NIRS
- NIRS-IVUS delineation of plaque architecture and composition has potential to enhance performance and improve safety of PCI
- The detection of vulnerable patients and vulnerable plaques
- The identification of patient requiring more intensive lipid lowering and anti-thrombotic therapy
- The accurate identification of lesion length prior to stenting
- The identification of lesions at risk of periprocedural MI
Guide catheters and wires
French size- The French scale (abbreviated as Fr) is commonly used to measure the size of a catheter or a sheath.
- French scale was devised by a Parisian maker of surgical instruments, Joseph-Frédéric-Benoît Charrière (1803-1876).
- French size ÷ 3 = diameter of catheter/sheath in millimetres.
- 6 Fr → (6÷3) = 2 mm
- 9 Fr → (9÷3) = 3 mm
- Definition of French size
- guide catheter outer diameter measurement
- sheath inner diameter measurement - The bigger the French size, the larger is the diameter.

Technical points to note when using the “anchoring technique”
- Take care not to perforate or dissect the side branch.
- For anchoring balloon technique, the guiding catheter must be big enough to allow dual balloon passage.
- For a 6 Fr guiding catheter, two low-profile monorail balloons can be used. Most 6 Fr guiders cannot accommodate a combination of a normal profile OTW balloon + one monorail balloon.
- In complex PCI (e.g., CTO PCI), a ≥ 7 Fr guiding catheter is recommended if anchoring balloon is to be used in combination with either a OTW balloon, or Tornus (‘anchoring Tornus technique’) device.
- Beware of possible stent damage / distortion / dislodgement when using anchoring balloon technique. Avoid excessive pushing of stent delivery balloon.
- Consider switching to other strategy if still encountering a lot of resistance.
Situation where ‘mother-and-child” double coaxial system is useful
- Provides coaxial alignment for increased backup support
- unfavorable vessel take-offs (e.g superiorly oriented RCA)
- anomalous arteries
- transradial approach
- other situations with guide catheter backs out
- Creates a pathway for balloon / stent delivery by providing greater flexibility and smooth surface
- calcified lesion – diffuse or ostial
- tortuous vessles
- distal lesions
- complex lesions
- CTO PCI
- facilitate the entry of retrograde guidewire into antegrade guide catheter
Complications of guidewire manipulation
- Plaque disruption and embolisation
- Arterial dissection and perforation
- Vasospasm causing acute closure
- Subintimal wire entry
- Wire fracture
- Wire tip entrapment
Balloon angioplasty technology
Balloon catheter systems- Monorail balloon catheters (SOE, Rx)
- Over-the-wire balloon catheters
- High-pressure balloon catheters
- Low-profile balloon catheters
- Balloon-expandable stent catheters
- Drug-coated balloon catheters (DCB)
- Porous balloon catheters
- Bifurcation balloon catheters
- Focused force (scoring) balloon catheters
Information supplied with balloon catheters in Europe
- Pressure-diameter curves
- Balloon diameter
- Shaft diameter
- Effective catheter length (without hub)
- Expiry date or use by date
- Indication of sterility
- Lot designation
- Instructions for use and warnings
- SI units
- CE certification
Balloon catheter parameters (typical measurements indicated, but these may vary with manufacturers)
- Balloon diameter (2-4 mm or more; low profile 0.85-1.5 mm)
- Balloon lengths (between 10 mm and 30 mm or more)
- Effective or usable catheter (length 140 cm)
- Proximal shaft diameter (2 French Monorail)
- Proximal shaft diameter (3 French OTW)
- Distal shaft diameter (2.5 French Monorail)
- Crossing profile
- Tip or catheter entry profile (0.017 inches)
- Nominal pressure (5-7 atm)
- Rated burst pressure (12-14 atm, high-pressure balloon 18 atm or more)
- Compliance (semi-compliant, high-pressure non-compliant)
Units (Data may vary depending on manufacturers or product lines)

Advantageous applications of OTW technology
- Total occlusion or tortuosity passage
- Distal wire exchange
- Distal drug or contrast medium injection
- Rotablation
- Septal ablation
Possible balloon-related complications
- Plaque rupture/dissection
- Stent loss
- Vessel occlusion/thrombus
- Balloon rupture
- Balloon trapping
- Balloon shearing off
- Coronary embolilsation
- Systemic embolisation
Bioresorbable scaffolds
Current concerns and possible solutions- Drug-eluting metallic stent platforms significantly reduced the amount of neointimal hyperplasia and associated clinical repeat revascularisation rate, but there are still concerns over late stent thrombosis, a persistent inflammatory reaction, incomplete endothelial coverage and impaired vasomotion distal to the stented segment, presumably due to residual drug, durable polymers and permanent metallic cage
- Fully resorbable scaffolds have a potential to solve these drawbacks of drug-eluting stents
Potential advantages of fully bioresorbable scaffolds includes:
- A reduction in late/very late stent thrombosis
- A return of the vessel’s vasomotion, adaptive shear stress and late luminal enlargement
- A reduction in bleeding
- An improvement in future treatment options such as bypass grafting
- Diagnostic noninvasive imaging follow-up with MSCT or MRI
The terms in question
- “Bioabsorption” stands for the disappearance of a compound into another substance, but does not necessarily mean “biodegradation” or “elimination of the polymer from the body”
- “Bioresorption” stands for total elimination of polymers from the body by excretion and assimilation after complete cleavage of macromolecules up to small molecules
Drug-coated balloons
Drug coated balloons- Drug coated balloons (DCB) represent a clinical treatment modality for local drug delivery in coronary and peripheral artery disease without the need for a temporary or permanent implant
- Advantages include a homogeneous drug delivery to the vessel wall, an immediate drug release without the use of a polymer, the option of using balloon catheters alone or in combination with a stent, no foreign object left behind in the body, and the potential of reducing antiplatelet therapy
Drug types
- A variety of different drug coated balloon concepts have been tested in preclinical trials. Most of the devices are coated with paclitaxel
- Excipients and the coating process play a major role in the physiochemical properties. Therefore, a class effect cannot be assumed
Clinical evidence
- Data from randomised clinical trials identified the treatment of coronary ISR as accepted indication for DCB (ESC guidelines class 1 level A recommendation)
- In coronary de novo disease, a strategy of DCB only angioplasty fulfills the requirements of the concept of ‘leaving nothing behind’.
- DCB are becoming the standard of care in femoro-popliteal arteries. However, there is no class effect.
Calcified coronary lesions
Mechanisms of action- Rotational atherectomy performs plaque ablation mostly by abrading inelastic and calcified plaques
- A less aggressive protocol of rotational atherectomy results in a lower risk of complications: burr-to-artery ratio of less than 0.7, a rotational speed between 150,000 and 180,000 rpm, and a pecking motion of the burr
- Optimal platelet inhibition is crucial to prevent or reduce the risk of thromboembolic events during rotational atherectomy
Directional atherectomy
DCA equipment and technique- Flexi-Cut™ and SilverHawk™ are the currently available and utilised devices
- Flexi-Cut™ uses an external balloon to establish vessel contact while the SilverHawk™ uses a lever system to bring the device in contact with the lesion
- Performing DCA correctly and safely requires formal training with direct supervision as incorrect usage can lead to major complications
- Correct guiding catheter choice and manipulation as well as the usage of support guidewires are essential for safe and effective DCA
- DCA should be avoided in heavily calcified or extremely angulated lesions
Performing optimal atherectomy
- Adjunctive angioplasty after DCA results in better immediate angiographic results and can convert suboptimal DCA into optimal DCA
- Currently, DCA is almost always followed by stent implantation
- IVUS plays an important role in the correct sizing of the device according to the vessel size as well as in the characterisation of the plaque
- DCA works only when the operator uses the device to achieve significant plaque removal and optimal lumen expansion, i.e., optimal atherectomy
- Optimal atherectomy has been defined as an angiographic residual stenosis ≤15%
- When performing DCA, initial cuts should be directed towards angiographically apparent plaque (as guided by multiple orthogonal views)
Clinical studies on DCA
- CAVEAT-I and CCAT compared DCA to balloon angioplasty and both utilised a non-aggressive debulking approach
- OARS, BOAT, ABACAS and START were registries using IVUS-guided optimal DCA, which resulted in lower restenosis rates than those in CAVEAT-I and CCAT
- SOLD, ADAPTS, AtheroLink and ADAPTS were the first registries to evaluate DCA followed by bare metal stenting which demonstrated encouragingly low restenosis results and led to the initiation of two randomised trials (AMIGO and DESIRE)
- AMIGO randomised 753 patients with de novo or restenotic lesions to DCA+stenting vs. stenting alone. No significant difference in restenosis and optimal debulking was performed in only 26.5% of patients
- DESIRE randomised 500 patients to DCA+stenting vs. stenting alone and also failed to show a clinical benefit from DCA
- A meta-analysis of these trials showed that DCA was associated with significantly lower restenosis and revascularisation rates
- There are only 2 registry studies evaluating DCA debulking prior to DES implantation which both show very promising results in left main bifurcation lesions
- In summary, the available evidence indicates that DCA does not improve late angiographic outcome when performed before bare metal stent implantation unless optimal debulking is achieved and relatively higher risk lesions are treated
Avoiding procedural complications with DCA
- Avoid dissections by careful guiding catheter manipulation without deep seating or over-rotation, not overinflating the urging balloon, and not performing cuts on angulated segments
- No-reflow usually occurs when performing DCA in vein grafts or thrombus-containing lesions and can usually be resolved with intracoronary vasodilators
- Side branches may become occluded during DCA but correctly performed DCA at a bifurcation can also be used to salvage side branches
- Coronary perforations can occur due to cuts on extremely angulated segments or from the distal guidewire. Although this complication is rare, it is imperative that PTFE-covered stents are available when planning to perform DCA
Favourable anatomical settings for DCA
- Ostial lesions
- Bifurcation lesions
- Left main lesions
- In-stent restenosis
Laser therapy
Mechanisms of ELCA- Photochemical mechanisms that ablate inorganic material
- Breaking of molecular bonds
- Generation of fast-expanding and imploding vapour bubbles creating dissections or even perforation especially when ELCA is activated in blood or contrast medium
- The Dotter effect
Essentials of the ELCA procedure
- Obtain good guide catheter support
- Choose guide catheter sizes according to the planned ELCA catheter size
- Secure correct guidewire positioning in the vessel lumen
- Allow a laser unit warm-up time of five minutes
- Choose ELCA catheter diameter to vessel diameter ratio of 0.5 to 0.6
- Flush guide catheter with at least 10 to 20 mls saline before laser activation
- Start with low fluence of 45 mJ/mm2 at a repetition rate of 25 Hz and increase if necessary
- During laser activation flush guide catheter with 1 to 2 ml per second
- During laser activation advance ELCA catheter slowly (0.5 to 1 mm per second)
Potential indications for ELCA
- The undilatable lesion
- CTO with successful wire crossing
- (diffuse) in-stent stenosis
- Thrombus-containing lesions
- Saphenous vein graft lesions
